- Feeling that others are picking on you or are trying to cause you harm.
- Having a feeling that people or things are "unreal" or experiencing episodes of feeling "zoned out" or "numb."
- Feeling emotionally dead inside.
"They (Borderlines) have the thinnest skin, the shortest fuses and take the hardest knocks. In psychiatristsí offices, they have long been viewed as among the most challenging patients to treat." Shari Roan
"We are not responsible for how we came to be
who we are as adults. But as adults we are responsible for whom
we have become and for everything we say and do."
from BPDRecovery
website
Jerold Kriesman and Hal Straus refer to borderline personality disorder as 'emotional hemophilia; [a borderline] lacks the clotting mechanism needed to moderate his spurts of feeling. Stimulate a passion, and the borderline emotionally bleeds to death.'
Is It Really A Crisis?
Tragic warning in suicide note
Another resource on suicide awareness www.learnpsychology.org
Intermittent Exploding Disorder: RECKLESSNESS
Co-dependency
DBT Treatment Reduces Suicide Attempts
Severe Suicide Warning
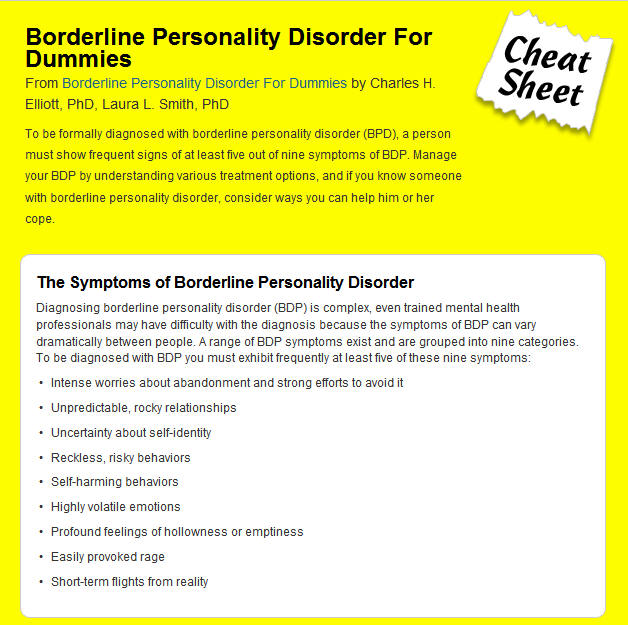
Borderline Personality Disorder Diagnosis: DSM-IV Diagnostic Criteria
A pervasive pattern of instability of interpersonal relationships, self image and affects, and marked impulsivity beginning by early adulthood ** and present in a variety of contexts, as indicated by five (or more) of the following points 1-9. The link of "Video" takes you to a video, all made by the same BPD patient. She explains the criterion in a very straightforward manner. I recommend viewing them.
1) Frantic efforts to avoid real or imagined abandonment. (Excludes #5)
2)
A pattern of
unstable and intense
interpersonal relationships
characterized by
alternating between
extremes of idealization and
devaluation.
3)
Identity disturbance:
markedly and persistently
unstable self-image or sense
of self.
4) Impulsivity in at least two areas that are potentially self-damaging e.g., spending, sex, substance abuse, reckless driving, binge eating. (Excludes #5)
5) Recurrent suicidal behavior, gestures, or threats, or self-mutilating behavior. Why is suicidality so common in Borderlines?
6) Affective [mood] instability.
7) Chronic feelings of emptiness. They may feel unfairly misunderstood or mistreated, bored, empty, and have little idea who they are.
8) Inappropriate, intense anger or difficulty controlling anger (e.g., frequent displays of temper, constant anger, recurrent physical fights).
9) Transient, stress-related paranoid ideation or severe dissociative symptoms.
Important Considerations about Borderline Personality Disorder
1) The 5 of 9 criteria needed to diagnose the disorder may be present in a large number of different combinations. This results in the fact that the disorder often presents quite differently from one person to another, thus making accurate diagnosis somewhat confusing to a clinician not skilled in the area.
2) BPD rarely stands alone. There is high co-occurrence with other disorders.
3) BPD affects between 1 - 4% of the population. The highest estimation, 2 %, approximates the number of persons diagnosed with schizophrenia and bipolar disorder.
4) Estimates are 10% of outpatients and 20% of inpatients who present for treatment have BPD
5) More females are diagnosed with BPD than males; reportedly by a ratio of about 3-to-1, though some suspect that males are under-diagnosed.
6) 75 % of patients self-injure.
7) Approximately 10% of individuals with BPD complete suicide attempts.
8) A chronic disorder that is resistant to change, we now know that BPD has a good prognosis when treated properly. Such treatment usually consists of medications, psychotherapy and educational and support groups.
9) In many patients with BPD, medications have been shown to be very helpful in reducing the severity of symptoms and enabling effective psychotherapy to occur. Medications are also often essential in the proper treatment of disorders that commonly co-occur with BPD.
10) There are a growing number of psychotherapeutic approaches specifically developed for people with BPD.
Results of the author's
test results from
similiarminds.com
|
Personality Disorder Test Results
|
Personality Test by SimilarMinds.com
Borderline personality
disorder Ďnot linked to
psychosis transitioní
By Mark
Cowen, Senior MedWire
Reporter
The presence of borderline personality disorder (BPD) is not associated with an increased risk for transition to full-blown psychosis in ultra-high risk (UHR) patients, research shows.
The authors found that there was no significant difference in 24-month psychotic outcomes between UHR patients with and without BPD.
"Clinicians working in UHR clinics have often seen Axis II features as co-morbidity, rather than risk or protective factors per se. This is in contrast to Axis I disorders, such as depression, that have often been implicated in increasing the risk for transition to psychosis in the UHR group," comment Andrew Thompson (Centre for Youth Mental Health, Parkville, Victoria, Australia) and team.
"Our findings support this distinction but we do not suggest that BPD pathology should be ignored as a clinical problem in its own right," they add.
The researchers studied 96 patients deemed to be at UHR for psychosis due to the presence of attenuated psychotic symptoms within the previous 12 months, a history of brief self-limited psychotic symptoms in the previous 12 months, or a genetic vulnerability to psychotic disorder with either schizotypal personality disorder or family history of psychotic disorder in a first-degree relative.
Of these, 48 developed full-blown psychosis over a follow-up period of 24 months, with no significant difference among the groups regarding at-risk criteria met, or functioning level at baseline.
Overall, 14.6% of the participants met DSM-IV criteria for BPD at baseline.
The researchers found that there was no significant difference between patients who did and did not develop full-blown psychosis regarding the presence of baseline BPD rates.
There were also no significant differences between the groups regarding the number of BPD traits.
"It appears that UHR patients with concurrent BPD pathology experience similar psychotic outcomes to those without BPD pathology, at least over the short term," conclude Thompson and team.
Licensed from Medwire news with permission from Springer Healthcare Ltd. ©Springer Healthcare Ltd. All rights reserved. Neither of these parties endorse or recommend any commercial products, services, or equipment.
Codependency and Borderline
Personality Disorder
(from
downwardspiralintothevortex.com
Blog by "Haven")
ďI canít live without him.Ē ďEverything will be ok as long as she loves me.Ē ďI must do everything I can do make sure that heís happy {and therefore associate me with being happy}Ē
Sound familiar?
Iíve been talking about relationships a lot lately so I thought Iíd touch on a couple things that are not uncommon with Borderline Personality Disorder: Codependency and Counter-Dependency.
I am not {generally} codependent so Iím relying on my research here. I am counter-dependent. Theyíre definitely both worth looking at.
When everything you do, when everything you think about saying {or not}, when everything you feel, is dependent on someone else, itís a problem. Itís codependent.
Codependent behaviors, thoughts and feelings go beyond normal kinds of self-sacrificing or caretaking. People who are codependent often take on the role as a martyr; they constantly put other's needs before their own and in doing so forget to take care of themselves. This creates a sense that they are "needed"; they cannot stand the thought of being alone and no one needing them. Codependent people are constantly in search of acceptance. When it comes to arguments, codependent people also tend to set themselves up as the "victim". When they do stand up for themselves, they feel guilty.
Codependency is an addiction. An addiction to people. Often very specific people. Codependency is a behavioural and psychological condition in which a person sacrifices his/her own wants and needs in favour of someone elseís wants and needs in order to maintain an unhealthy relationship. Codependency is probably related to the intense fear and frantic efforts to avoid abandonment common in BPD.
Codependency is a dysfunctional relationship with the self. It involves habitual behaviors that are ultimately self-destructive. Having some symptoms or periods of codependency are actually pretty common for most people. But in order to be considered a true codependent, like any disorder, it is something that must persist for an extended period of time and disrupt your life in an unhealthy way.
So whatís the difference between depending on someone and being codependent on someone? In a healthy relationship a person can recognize when they need help or assistance in life. Having someone you trust and can turn to for occasional assistance or help when you need it, but otherwise being able to manage your life and support your own self esteem on your own, is a healthy level of dependence. To be codependent is to forget that your life and self-esteem will go on without the love and support of the person you are counting on. Everything in your world, your happiness, yourself worth, depends on the thoughts, opinions, and emotional integrity of the person that you are focused on.
A codependent Borderline lacks a true self-perception. Their identity is dependent on the people around them. Who they are is determined by the perception of someone else.
There is a hidden motive in the actions of those that are codependent. One so sneaky that the person themselves are usually unaware of it. Like many aspects of BPD, itís a motivation of selfishness. When someone is lost in a world of codependence, sacrificing every waking moment to ensure the happiness of those around them, the real underlying, subconscious motivation isnít because they altruistically want the world to be happy. No, itís because they want to be loved and appreciated. Everything they do stems from the motivation of wanting to receive: receive love, receive validation, receive self-worth, receive, receive, receive.
To be fair, most people do this to some extent. We do things because ultimately it is to our benefit to do them. Itís that nature of the beast of humanity. For a codependent relationship though itís so prevalent in the personís life that it utterly disrupts their ability to live in a healthy way.
On the surface they appear to be the pinnacle of giving, caring, and nurturing, and indeed all those actions are, they often give of themselves to a faultÖ but itís at the expense of what they really need, which is acceptance by themselves. Everything they do is to gain validation from an outside source.
Someone who is codependent will often bear the burdens of the person they are dependent on. Their mind will be consumed with thoughts of how to provide happiness for someone else. Their happiness, their feelings will in fact, be determined on whether or not something they do is able to create happiness in another. Relief comes from seeing relief in another. Self-worth comes from the recognition in another that what they did made their life better in some small way. This is where I have found myself being codependent before.
The ironic thing is that because someone who is codependent is so absorbed in being accepted by another, they are actually incapable of being accepted by another because they arenít providing anything real for another person to accept. Theyíre giving and giving and giving, but theyíre giving things that they think another person wants, not things that they actually are.
How can you feel secure in the love of another human being when ultimately you canít believe that they love you for who you areÖ Because all youíve shown them is what you can do for them and not who you can be with them? Itís an innate contradiction that someone who is codependent may never see. They give things, they give actions, they give relief of responsibility, but what they arenít giving is the one thing they really need to give in order to form a true bondÖ themselves. But since their own identity is based on the perception of the person theyíre trying to please it becomes a self-fulfilling cycle of sadness, self-doubt, and resentment.
Also ironically, is that the actions of a codependent often contribute to their partner being selfish and self-serving instead of appreciative and nurturing, which is what they want. When everything you do is focused on another person, naturally their focus is going to turn more and more towards themselves as well. The codependent may subconsciously condition their partner to also believe that everything that is done should be done for them, which contributes to their partner ignoring the needs of the codependent, and makes the codependent redouble their efforts to gain attention and favor, leading to the partner becoming more self-involvedÖ. Can you see where this is going? It doesnít help cultivate a healthy relationship at all. All it does is cultivate an environment where nothing is ever enough and the codependent person will continue to lose themselves to a cycle that they can never find the security they need.
How can
you tell if you are
codependent? There are many,
many symptoms of
codependency. I didnít come
up with this list, in fact I
found the write up for most
of this here. I will take a
look at how I think these
things line up with my life
though. So letís take a look
at some of them shall we:
Symptoms:
Care
taking: the codependent
individual feels responsible
for other people. S/He feels
anxious and even guilty when
another has a problem. S/He
feels compelled to help that
person solve their problem.
S/He anticipates the other's
needs and feels angry when
his help is not effective or
rebuffed. At the same time,
the codependent feels
slighted that others won't
help her/him out when s/he
needs help. However, this
same individual who is
constantly doing way too
much for others, and not
getting "any" help from
anyone, will usually answer
when asked what is wrong or
what do you need, responds,
"Oh, nothing." The
codependent minimizes
his/her own worth. The
codependent is his/her own
worst enemy.
I can
definitely see myself having
a lot of these codependent
care taking traits. Wouldnít
you feel slighted if you
helped someone out
constantly and they didnít
reciprocate at all?
The codependent is over committed, harried, pressured, feels safe when giving, but insecure when someone gives to him/her, goes out of her/his way to help others, and believes deep inside that other people are responsible for the way they are and will blame others for the "spot" they are in. Others make them feel the way they feel, they are victimized, angry, unappreciated, and used. Others are driving them crazy.
Over committed, harried, pressured, feels safe when giving: Check. Iím not at all insecure when people give something to me. In fact I usually keep these things around me to help with my lack of object constancy. I do feel weird when someone goes out of their way for me, but I think thatís more because Iím so unused to it and also detached from my emotions that I donít always know how to respond properly. ::laughs:: Believes deep insideÖ. No no, I believe right up on the surface there that most people are responsible for the ďspotĒ theyíre in. I can absolutely recognize and accept when people have been truly taken advantage of and given a bum lot in life, but ultimately we are responsible for our own lives, choices, and actions. I may have been born and abused into this slew of mental health disaster, but itís my responsibility to do something about it. Others are driving me crazy. Hah! True.
Low Self Worth: codependents tend to come from troubled, dysfunctional families, and will deny this to the very end. They blame themselves for their family's shortcomings. They blame themselves for everything. They pick on themselves constantly: not intelligent enough, not pretty enough, not smart enough, not athletic enough, not good enough. But if another criticizes them, boy do they get defensive and angry, not to mention self-righteous. Don't try to give a codependent a compliment; they reject all compliments and praise, even though they get depressed from lack of compliments and praise. They feel "different" from the rest of the world. They reject themselves, but fear rejection. Everything is taken personally, they love being the victim (though will deny it with their last breath). They have been victims of sexual, physical, or emotional abuse, abandonment, neglect, and/or alcoholism. They feel like victims, carry lots of guilt and shame, and think their lives are not worth living. They should have done this, should have done that. They "should" themselves to death. Codependents say, "Why me?" on the outside, and know "why me" on the inside. While trying to prove to others that they are good enough, to themselves they feel worthless and empty.
My
self-worth fluxuates with my
mood or to be perfectly
honest, my body image. My
self-worth is entirely
dependent on how I perceive
myself and this ties in
immensely to my dysmorphic
issues and my personal
accomplishments. Whether
anyone else recognizes what
I do or not does not raise
or lower my self worth. In
fact, having my achievements
recognized often makes me
feel awkward because I donít
want the attention. I am
very hard on myself, I do
put myself down, but this is
due to my perfectionistic
nature. Criticisms will make
me spin down emotionally
because it is a recognition
that someone else has seen
my flaws. I raise and lower
my self-worth. I can usually
take compliments.
Compliments from women I
take sincerely. Compliments
from men that Iím involved
with I take sincerely
(especially if weíre already
sleeping together because
itís not like they have to
butter me up to get what
they want now). Compliments
from men I am not close to
or strangers, does make me
question their motives. Big
time. This has been proven
to be an issue though and I
donít know if itís just me
being paranoid or me being
justified. Maybe a bit of
both, but it doesnít mean
that Iím wrong to question
peoples motives. I do feel
ďdifferentĒ from the rest of
my world, but I actually am
different than most people I
know. Life is definitely
worth living even if it
sucks sometimes. I do
ďshouldĒ myself to death
sometimes but I do this
regardless of whether
something is just for me or
not. ďWhy me?ĒÖif I know it
on the inside than thatís
all there is to it.
Repression: most codependents repress their own needs, their own desires. They are afraid to let themselves be who they are and often appear rigid and controlled. They repress all thoughts of self-worth out of their awareness and they are full of guilt. Codependents cannot have fun.
I definitely repress my own needs and desires in order to take care of those around me first, but that falls into the care-taking category. If itís just me on my own I donít do this. If I need something I definitely go ahead and take care of whatever it is. Growing up and until a year or two ago I felt guilty about getting myself anything that I desired, but Iíve pretty well taken care of that at this point. I can definitely have fun too.
Obsessive Compulsive Disorder: codependents worry. They worry about the slightest and silliest things (True): they worry that people are talking about them (False); they worry that people are not talking about them (False); they lose sleep over little things (True); they check up on others (Rarely); they try to catch people in the act (Only if I know Iím being used, manipulated, taken advantage of or plotted against. i.e. Evil-Ex); they never find any answers (False), they focus on other's problems (True); they spend money compulsively (I make some compulsive decisions but only if all my bills and responsibilities are taken care of first); eat or drink compulsively (True) ; and wonder why they have no energy and why they never get anything done (I get so much done itís ridiculous).
My OCD tendencies have nothing to do with codependency and everything with needing structure and control in my life. Iím not even sure how most of these things qualify as OCD.
Controlling Behaviors: codependents try to control events and people through helplessness, guilt, coercion, threats, advice-giving, manipulation, or domination. They are afraid to let people be who they are or let events happen naturally. They've lived in so many situations in which they had no control (abuse, alcoholism, etc) that they now try to control everything and get frustrated and angry when they cannot. They end up feeling controlled by events. They feel controlled by others. They resist change as if change were a contagion.
This is
one thing Iím pretty happy
to say that I donít do. When
I was younger and Acted Out
I definitely had more
manipulative tendencies that
I would consider controlling
behavior. After Evil-Ex
though, I learned to let go.
With him I definitely felt
the need to control a lot of
things, but he was actually
working to make my life spin
out of control. I donít hold
onto things as hard anymore.
I do resist change. Change
is hard. Especially when it
comes fast it can
destabilize me, but I donít
know if that is codependent
so much as normal. The most
zen of Buddhist monks will
never have a problem with
change, but everyone gets
thrown for a loop when
things change unexpectedly.
I used to fight change tooth
and nail. Iíve learned to
adapt and move with change
as much as I can though. The
only person I am compulsive
about controlling, is
myself. No matter how you
look at it, this just isn't
going to work.
Denial: codependents ignore
problems or pretend they do
not exist. They pretend
things are not as bad as
they are; they tell
themselves it will get
better; they stay busy to
avoid thinking about things;
they get confused, sick,
depressed and visit doctors
for a prescription. Many are
workaholics. They lie to
themselves and others. They
believe their lies. And most
of all, codependents will
leave a healthy situation
(by lying to themselves that
it was an unhealthy
situation) and get back into
an unhealthy situation;
though for the most part,
most codependents either
never leave an unhealthy
situation/relationship, or
they go from one unhealthy
situation/relationship to
another.
Denial is one place Iíve struggled with, but itís always been a wanting to believe something even though I knew it to be otherwise. Even when I was with Evil-Ex I knew the truth of my situation, but my emotions were in such complete opposition that I couldnít reconcile the two. Thatís what made it more maddening for me. I saw the reality but felt a different way. Iím very good at seeing what is actually going on. Making a decision in opposition to my emotions though can be difficult for me. There were times I wanted to believe his lies, but I didnít actually believe his lies.
Dependency: codependents do not feel happy or content with themselves. They look to others to supply them their happiness or their needs. They are threatened by the loss of anything or any person that provides them with their happiness.
They do NOT love themselves. They did not feel loved by their parents. They equate love with pain and believe others are never, ever there for them. They need people more than they want them; their lives revolve around someone else's life; they tolerate abuse; feel trapped; leave one bad relationship and jump into another bad relationship. They wonder if they will ever find true love. And if they do find true love, they will leave that and find a loveless relationship because deep inside (often beneath consciousness) they feel unworthy of love.
Hm. I donít expect or think anyone else can make me happy. I do know that I am happier when I am with people I care about and enjoy the company of. Left alone for long periods of time (days, weeks, months) I do sink into a depression greater than usual. To me this doesnít seem unreasonable though. Who wants to be forever alone? Some people Iím sure, but that strikes me as more unnatural. I think Iím more concerned with being alone, than being happy.
I do equate love with pain, but every experience of romantic love Iíve had has actually caused me deep and intense pain. This is a result of experience, not unfounded fear. I actually do not tend to jump from one bad relationship to another. This constant dating and always having a new partner is relatively odd for me. Traditionally I will end a relationship and stop dating for 6-8 months so I can get my head back on straight. With only a couple exceptions the people I choose to date are generally very good people. Then again, those donít seem to be the ones I form intense attachments to, do they.
Poor Communication Skills: codependents blame, threaten, coerce, beg, bribe, and advise others. They don't mean what they say and don't say what they mean. They don't take themselves seriously and expect others to do the same. They avoid getting to the point, asking indirectly for attention by sighing, crying, or moping around. They say everything is their fault. They say nothing is their fault. They can't get to the point, and if pressed, they're not sure what the point really is. They believe their opinions do not matter and have difficulties asserting their rights or expressing honest emotions, openly and appropriately. They apologize for bothering people.
Iím getting better at communicating my needs though in the past I was very, very bad at stating anything that was going on with me internally. I do often feel guilty for expressing what is on my mind though I donít believe things are my fault when they actually arenít. Iím also absolutely ok with acknowledging when I have screwed up and taking the blame for something Iíve doneÖ once I recognize that I screwed up. Itís so tricky. For a long time I blamed myself for the abuse I took in my relationship with Evil-Ex because I felt responsible for staying in that relationships. To an extent I still feel that is my fault even though the abuse didnít end once I stopped the relationship. I thought it was my fault. In reality though, I didnít ask for the abuse, he had no right to treat me that way. It was his fault for being a monster. Tricky tricky tricky.
Poor Boundaries: codependents say they won't tolerate something from anyone, and then engage themselves in exactly that. Then they gradually increase their tolerance levels till they can tolerate most anything others do to them. They allow others to hurt them, over and over and over again. They stay in bad relationships for all the wrong reasons: to fix the other; for the kids (like kids need to grow up in a loveless relationship); because things will get better; and worst of all: because they feel they deserve to live in hell. They complain and blame but far too many never get away from their abuser. Then they finally get angry and become totally intolerant and the cycle begins all over again.
Iím definitely guilty of saying I wonít tolerate something but then allowing it to happen. However, this is conditional. If itís someone that Iíve already fallen in love with and have emotions that are beyond my ability to control than this becomes a possibility. If itís not someone that Iíve fallen for and do not have a deep attachment to, then I wonít tolerate shit and I can put up reasonable boundaries. I donít have any of these reasons though. If I stay with someone that is hurtful itís because I love them, not because I believe I donít deserve to be happy. This may still be an expression of codependency, b/c the thought of losing someone Iím so attached to is beyond painful. However once I reach my limit, Iím done. For good.
Lack of Trust: codependents do not trust themselves, their feelings, their decisions, other people, or even God. And then, right out of the blue, they'll trust someone who is totally untrustworthy.
I donít trust people for good reason. I donít trust myself because I tend to be impulsive and I make poor emotional choices. However! I do trust some people that have most definitely earned my trust, like Roommate or my sister. One thing Iíve never done is trust someone that is totally untrustworthy. I may interact with them, I may want to trust them, but I wonít actually trust them.
Sexual Problems: codependents go through cycles in the bedroom. They are caretakers there too. They have sex when they don't want to or withdraw sex to punish their partner. They try to have sex when they are hurt or angry, and refuse to enjoy it. They withdraw emotionally from their partner, feel revulsion toward their partner, and don't want to talk about it. They reduce sex to a technical act, wonder why they don't enjoy it; lose interest; make up reasons to abstain, wish their partner would die, go away, or guess what is wrong with them; they have strong sexual fantasies about others and consider having affairs.
I can definitely see myself being a caretaker here. I never say Ďnoí to sexual anything even when Iím tired or uncomfortable (if itís with someone that Iím already established with! I donít sleep with random people). Though to be fair I do actually enjoy it and I think using sex or denying sex as a weapon or punishment is just wrong. Idk, I have very few sexual boundaries because I really do enjoy a lot of things in regards to sex. Itís something to enjoy and have fun with. When my boundaries were violated I did learn to talk about it and set solid boundaries!
General: codependents can be extremely responsible or irresponsible, they become martyrs, sacrificing their own happiness. They find it difficult to be happy, feel close to others, or have fun and be spontaneous. They are passive aggressive, feeling passive, hurt, helpless yet violent and angry. They laugh when they want to cry. They are ashamed of their families, of their relationships. They cover up, lie, and protect their family from their problems. They don't seek help because they don't feel the problem is all that bad. And then they wonder why the problems never go away.
In general I can see much of this as true for me. Iím not usually ashamed of my family or relationships (unless cognitively I know the relationship is very unhealthy and yet Iím still emotionally attached). When it comes to my problems, I definitely feel shame when I am not able to take care of something on my own and will not ask for help if I can avoid it. I donít want others to see me struggle. I think there is an important distinction in this statement. That being ďTo protect their familyĒÖ. I may cover up and lie about having problems, but itís not to protect others, itís to protect myself.
I would think that someone who is codependent would feel helpless, feel that they needed someone else to rely on in order to fix their problems. Maybe thatís wrong though. Maybe someone that is codependent is so worried about people thinking they will be too much trouble if they have any problems that they must hide them. What do you think?
Over-responsibility Ė is taking responsibility for someone elseís problems. A person who is over-responsible will blame themselves for the actions, feelings, and thoughts of others. This can make them a victim of the problems other people have regardless of whether or not those problems have anything to do with them.
No. I often feel guilty if I canít help enough but I donít usually feel responsible for other peopleís problems.
Resentment and self-pity often accompany co-dependence. When you do so much for other people (whether voluntarily or involuntarily), itís easy to feel unappreciated, resentful, and self-pitying when you do not receive acknowledgement for the things you do.
I donít know folks. I recognize a lot of these traits in myself, but I donít know if I necessarily attribute all these things to codependency. A lot of them come from issues that I have that are completely separate from having anything to do with relationships. Or theyíre a product of abuse. Thatís the problem with self-diagnosis. You can go through a checklist and see that you match certain things, but if the context of those symptoms isnít right then you may be attaching to a false label.
Top
Borderline Personality
Disorder: Erotic
Transference
By Sonia Neale
Ahh, the Erotic Transference! The question is do we want to have sex with our therapist because of a deep-seated oedipal complex, primary attachment gone tragically awry, a pre-verbal object relationship that cannot be unified or do we simply want to shag an attractive, empathic person who sets our genitals on fire?
Much psychological literature is written by Sheldon Cooper types (The Big Bang Theory) who are socially autistic or have Aspergerís syndrome and are desperately trying to quantify the unquantifiable by using terms such as ďerotic transferenceĒ instead of ďlust or loveĒ because by using wholly scientific terms it distances themselves from their own primal and lustful urges. That is why Amy Farrah Fowler (Sheldonís girlfriend) cannot understand these sinful longings she gets when she is around men. It greatly distresses and frustrates her.
Admitting you have sexual feelings for your therapist to your therapist can create shame and disgust. We are all sexual beings, itís how we relate beneath the superficial veneer of expected manners and mores of society.
Civilization as we know it would break down if we all gave in to our primal urges, so we stifle them down until we get into an intimate relationship with someone. Unfortunately that someone can be a professional business person in the form of a clinical psychologist rather than a hot guy/girl at a nightclub where both parties know that the end result of the night in question can end up with a roll in the hay. That is not an expected outcome of the therapeutic relationship, yet the feelings can be there Ė from both sides of the couch, the other side of which is known as erotic counter-transference.
Just because you want to have sex does not mean you should have sex, but does acknowledging these feelings help the situation any? Is it the man or woman of the therapist that turns you on, or is it the warm intimate association of sharing secrets in a cozy, isolated office?
If you saw your therapist at the beach in a pair of baggy bathers or sitting at the pokies in the local casino, or face down in the frozen chip department at the local supermarket would that not shatter your illusion that they are some sort of Greek God sent down from Mount Olympus just to save you from yourself?
Many if not most therapists are very uncomfortable with their clientís ďerotic transferenceĒ and find it difficult to talk to them about. This is understandable. People with Borderline Personality Disorder with serious boundary issues and greatly heightened emotions and high sensitivity tend to fall in love easily with anyone who shows them small tender mercies. I know this equation so intimately.
My therapist gave me space and time to explore these feelings and never made me feel ashamed of them. I just had to own them knowing she did not feel the same way. She made that crystal clear in a sensitive, caring manner. Thank God she did. I am a better person for her boundaries and ability to enable me to take responsibility for my feelings and deal with them without involving her. It was a long and messy process but one that clarified our relationship, gave it a framework and created guidelines for healing and moving on so I could live my life fully.
Dealing with this is something that desperately needs to be addressed in the training process of future therapists.
Sonia Neale started therapy
writing for
post-natal-depression and
anxiety. Fifteen years later
she is the author of two
books, The Bad Motherís
Revenge and Death by
Teenager, both published by
ABC Books/Harper Collins.
She lives in Western
Australia, is married with
three teenagers, has a
certificate in
Psychoanalytic Psychotherapy
and is studying for a
psychology/counseling
degree. She is not yet a
psychotherapist, and has
deferred her academic
studies in order to pursue a
Certificate IV in Mental
Health. She currently works
as a facilitator in the
mental health field. Her
website address is
www.sonianeale.com.
Borderline Emotional
Anaphylactic Reaction:
Mindfulness and Acceptance
By
Sonia Neale
Sometimes, the smallest things in life can cause the greatest pain and physical reaction. A beeís sting is almost invisible to the naked eye and yet can easily kill someone when they have an allergic reaction. A mere critical stinging comment can just as easily send a person suffering Borderline Personality Disorder into ďemotional anaphylactic shock.Ē
When a person has a life-threatening reaction to the poison from a bee sting, an ambulance is called and the person is taken to hospital where they receive treatment for their illness as well as respect and dignity but when someone suffering an emotional reaction to life circumstances presents at emergency, they are sometimes treated with rejection, intolerance and disdain. People can die from a bee sting and Borderlines can ďdieĒ from their own personal rage and self-hatred. If you present at emergency with a swollen face and throat unable to breathe with all your body organs shutting down, is some doctor or nurse going to say, ďOMG, itís a tiny bee sting, how bad can that be, look at you, get over yourself,Ē like they sometimes do when Borderlines present at hospital with similar symptoms.
Yet both types of people are in much pain and danger. One is considered entirely physical and the other is considered entirely emotional. Or is it entirely emotional? When a sensitive person with a history of trauma has an emotional ďbee-stingĒ reaction to someoneís criticism there is a definite physical reaction.
Borderlines tend to be hypervigilant, which means they live with permanent muscle tension and a certain excess of adrenaline pumping round their system at any given time. So when criticism hits, the body goes into an emotional anaphylactic state where cortisol floods the brain and body system and a type of blackout occurs where nothing anyone says or does registers. Your body has gone into ďshock.Ē When I used to get into such a state someone could have cut my arm off and I would not have noticed.
Things are said during this time that are simply appalling. I have used language I would not use in normal everyday life. I have said things that are deeply hurtful and as my husband has said, ďyou can mend a vase but the cracks are always there for those to see.Ē My therapist says it is best to repair those cracks with gold. Her favorite quote, by Barbara Bloom is ďWhen the Japanese mend broken objects they aggrandize the damage by filling the cracks with gold, because they believe that when somethingís suffered damage and has a history it becomes more beautiful.Ē I prefer her take on this matter.
Therapy has taught me that my perception of events and criticism is usually erroneous. Even if people are critical and disrespectful, it is about them and not me. If my ideas get criticized it is not because I am a loser and I deserve to die, it is because we both have a different belief system and ways of handling situations. There is no right or wrong, just opinions.
I have criticized my therapist on many occasions including recently when she raised her colleaguesí fees in the light of almost certain public benefit cuts. Her reply was that her practice survived before the benefits were given and hopefully will survive after the benefits are cut. She raised her fees because she valued herself and her colleagues. She did not feel the need to get upset or question herself or her actions because she believed that what she was doing was the right thing to do.
It is this sort of self-valuing that is empowering to people like myself who always feel others are more valuable and powerful than I will ever be. When we assert ourselves and say, ďNo, I donít like that becauseÖ.Ē we can start to realize that it is ok not to people-please all the time. I said no to unpaid overtime because I value myself as a worker otherwise I will feel undervalued and get resentful. Like my therapist I am worth it.
Mindfulness and radical acceptance of people and situations as in Dialectical Behavior Therapy is the key to, well, if not happiness, then a more content and peaceful self. It is the road to what Abraham Maslow calls self-actualization Ė autonomy, independence, few but deep friendships, a philosophical sense of humor, resistance to outside pressures and transcendence of the environment. These are the things I strive for and have spent much time in therapy trying to get a good grasp of.
A great book, which
promotes self-actualization
that I am reading at the
moment, is ďThe Art of
HappinessĒ by the Dalai
Lama. While I may not quite
reach the emotional plateaus
that His Holiness is capable
of, I can certainly learn
how best to inoculate myself
when swarms of emotionally
stinging bees are trying to
infiltrate my brain and body
system.
Top
Top