|
New
Visitors since May 2009
|
|
Website author was featured on PBS's "Second Opinion" show on
their Borderline Personality Disorder episode in 2016-17. |
|
Borderline Personality
Disorder
|
|
Designed
& Researched by Amy L.
Allison of Odyssey Design
|
|
|
|
A Webquest for Understanding This Disorder
Site Created by
Odyssey
Design Copyright ©
2009-2025 All Rights
Reserved
Terms
& Conditions
Website-wide revision September 2023
S tatement
of Purpose: To increase
mental health professionals' and
society's awareness of the
internal horror experienced by
people suffering with Borderline
Personality Disorder, and
treatments for their recoveries.
Borderlines diagnosed with the
disorder represent half of those
who suffer. The
remainder of the people are those
who experience the pain, insanity,
and self-doubt that result
from being in a relationship with
a BPD. The site is for both
groups, as well as for
professionals, to a lesser degree.
Approximately 1.5 - 6%
of
the people in the United States
are afflicted with this
disorder. In a psychiatric hospital
setting, they make up
40% of the patients.
The intent is
not to dazzle you
with a flashy website describing
Borderline Personality Disorder,
often called the "orphan
illness" of mental health.
This
webquest's main purpose is to give
you free information;
hopefully this will assist you in
making wise decisions and taking
positive actions. After reading the
famous book
Stop
Walking on Eggshells,
a psychiatrist told me that
without treatment for BPD
"people often die from it"...
with a suicide rate of 1 in 10
attempts. This disorder
can cause immense wreckage, and
there is an overwhelming
denial of how much destruction
it can truly cause. However, it is a
mis-understood mental health
problem...If
approximately 4 percent of the U.S.
population has it, that would
amount to about
11 million
people across the country. We've
heard about gluten intolerance
and rheumatoid arthritis, and
BPD occurs more often than these
maladies.
Why don't we
hear more about Borderline
Personality Disorder?
My realization that there was a need for researching and
designing a website of this
topic came to me in May of
2009; this website's main
objective is to educate others
on all facets of
this personality disorder
- diagnosis, treatment,
medication, therapies,
misconceptions, the patients,
their families, the therapists,
the psychiatrists, the stigmas,
to name a few. I
have not received
payment from anyone for
publishing this website. A lot of websites
about medical issues are
often either an overview, with a
synopsis of information, or they
may examine one issue in
depth. I have
attempted to cover almost
all
issues encountered with
BPD in a little more
detail. I
have searched the internet for
BPD resources, new
information and new
treatments; and I have
expanded this site on
a daily basis. I
might add that this is a huge
website. Take what you can use
and leave the rest.
Please bookmark this site. It is
user-friendly. Many, many
links will take you away from this
website, because of the volume of
related topics. You may
return to this site by just
hitting your "Back" button on your
browser. I encourage you to
bookmark other links, away from
this site, you find interesting so
that you may return to them
later.
I have
combed through the internet
searches (so you do not have to)
to bring you the most current
information published-- to
create a BPD portal, so to
speak.
My goal has
been to provide you with 'one
stop' where you may learn all
about the disorder, and with
the help of a professional,
determine your next
action, as a BPD or as the
family, friend or loved one. What I have
learned in researching this
baffling disorder, I pass on to
you. I hope that you will
do the same for others.
Share this website.
I
am encouraged by the number of new
people viewing this website, and
the repeat visits - the word is
getting out about BPD.
Please, just pass it
forward. My responsibility
to you is to pass on all the
information that I can
compile. In Google searches
of
Amy Allison on Borderline
Personality Disorder
Webquest search yields this
website 38 out of the first
54 search results.
This can change
from time to time.
I
was perplexed by how few
professionals and treatment
centers there are that are DBT-certified
to treat this disorder; more
are needed to address the growing
numbers of people who are
diagnosed with this
disorder. As I have
researched this topic for a year,
and took the DBT Skills course
13-15
years ago, I have discovered that
there are many, many therapies
that are being accepted and widely
used to treat BPD, with amazing
success! I also am aware of how
professionals limit the number of
BPD clients on their caseloads,
due to the exhausting nature of
professionally treating someone
with this disorder. I
understand their reluctance in
treating clients with BPD.
It is a thankless, grueling, and
draining experience, so I've
read. I can imagine.
Many
resources exist for people
with BPD, as well as for their
families, spouses, parents,
partners, friends, or
children (all called
Non-BPD's). If you
are in a relationship where
scenarios with this person have
evolved from being a bit
off-balanced to a gruesome
horror movie - or living with a
certain someone feels as though
you are creeping through a field
of land-mines (with the
possibility being blown to bits
at any moment), or you live your
life as if you are existing in a
burning Hell, you possibly could
be dealing with a person with
BPD.
Have you seen
the movies "Fatal Attraction"
and "Girl, Interrupted"?
Do yourself a favor, rent one or
both of these movies and watch
them. Yes, they will make
you very uneasy.
Maybe YOU can relate to those
portrayed, and wish to learn
more about why your life isn't
working. Please, don't
hide under a rock, or drown
yourself in alcohol, drugs or
food, sex, gambling or
look the other way, or
hope it will go away.
Trust me, it won't. As it
is heard in AA meetings:
"If you don't think you have a
drinking problem, then why are
you sitting in this
meeting?" What made
you examine this site? I
assure you, it is not as
entertaining as some, but you
will have a pretty good grasp
about the disorder when you
leave it (but hopefully to
return later.)
I will add
something to note: this
website has A LOT of information
for the non-BPD's as well.
Non-BPD's are those who live
with or deal with a loved-one,
friend, spouse, employer who has
this disorder of BPD.
Please see "Help for the
Non-BPD's" on the sidebar in the
upper left-hand of this
page.
You are
visiting this site because
someone, or you, have felt that
there was a reason for all the
trauma-drama in your life;
or the topic interests you. Or
you may be a professional.
They care. We care.
I care. I have lived
it. I have been to
OZ. I hope you consider
seeking some help.
Start
with this
website. It's
risk-free and FREE. 
The good news is - BPD is
treatable.
Your
pain brought you here;
Hope and Help in this website
will keep you
coming back. But--Keep
coming back.
!!
IMPORTANT CHART
BELOW !!
A diagram
of BPD, addiction and mental illness
statistics for the U.S.
Top
|
|
Thanks to
the internet and Google, I
am able to get new information
on this subject of BPD as it
is uploaded to the internet by
whomever. I receive
an immediate notification.
Anything newsworthy, I add it to
this site. It pays to be a
geek sometimes.
Top
|
|
Repeat
Visitors
This website is over
15 years old !
Created in
May 2009
Site Created by
Odyssey
Design
Copyright ©
2009-2025
Odyssey Design
-- All Rights Reserved
Criteria for BPD per
DSM-IV-TR:
(Must meet 5 of these
9 criteria)
1) Abandonment
fears
2) Intense,
unstable
relationships
3) Identity disturbance
4) Psychotic-like
perceptual distortions
5) Suicidal and/or
self-injury
6) Emotional
instability
7) Emptiness
8) Anger
9) Impulsivity
|
|
ANYONE
CAN HAVE
THIS DISORDER
|
|

|
An executive
Your boss
|
|
Young children
|

|
|

|
Some
members within a work-group |
|
A sportsman
|

|
| Maybe
you Maybe me |
|
70% are
female, 30% are male. These
%'s are changing-more males
are diagnosed.
|
|
|
DID
YOU KNOW? Robert
Schloesser and colleagues at the
National Institute of Mental
Health (NIMH) found that
an environment filled with
enriching activities could lift
your mood. Experiments in
mice showed that enriching
activity helped them to generate
new neuronal (brain cell)
growth...including cells and
pathways in the brain. It has
been concluded that you can
alter your mood by engaging in
activity.
|
|
52.2 % of
those who suffer from
borderline personality
disorder are addicted to
internet use.
That's what the studies
say.
|
|
|
|
...or all sorts of emotions
can overcome a
Borderline in a short
period of time....usually
without warning.
|
|
"A
Borderline has no emotional skin."
|
|
A
Borderline is beat up by their
own emotions.
|
|
Movies / Music Depicting
Borderline Behavior
"Her Smell" Guns & Rose inspired.
Borderline indie rock star
Documentary on BPD
Woods Hole Film
Festival
A musical entitled "Borderline"
played by a Borderline patient and
her real-life therapist.
Movies (whose main
characters have BPD):
Thirteen [2003] One of the
closest depictions of BPD
Fatal
Attraction - Glenn Close
[1987]
Girl,
Interrupted - Winona
Ryder [1999]
Silver
Linings Playbook
The Hours
Eternal
Sunshine for the Spotless Mind
Songs
(relevant for their
lyrics)
"Unwell" by
Matchbox 20 [2008]
"Borderline"
by Madonna [1984], depicts
emotions of this disorder
Top
|
|
 |
The
ball is
like
the BPD's emotions
|
| (Smilies
"talk". Mouse-over means place
your mouse over the smilies and
hold it there until the message
appears.) |
|
|
Tip: if the videos
scroll too fast to read all the
words on a page, push the
sideways triangle (right under
the video on the far left), and
it will turn into a "=".
This will pause the video. When
you are ready to continue,
press the "=" & the video
will start up.
|
|
|
.







|
Treatments
When
a person with BPD allows
themselves to be treated (denial
is often part of the disorder),
treatment generally consists of
medications and therapy.
“Up
until now, existing therapies
for BPD have proven to lead to
only partial recovery or have
only been able to reduce
self-harming behaviors.”
That has been rapidly changing
with the introduction of new
therapies.
Medications, (see
listing) which
are often successfully used to
reduce depression, dampen
emotional ups and downs, and
put the brakes on excessive
impulsivity. Antidepressants
can help with depression,
while mood stabilizers such as
Depakote, Tegretol, or Lithium
can help with mood swings.
Selective Serotonin Re-uptake
Inhibitors (SSRIs) such as
Prozac, Zoloft, and Paxil may
help control impulsivity, as
may Effexor, a related
antidepressant. Buspar and
Cymbalta are used to relieve
discomfort associated with
BPD. Tegretol may be
helpful for controlling
excessive anger and
irritability. Many
medications are used to treat
the symptoms and discomforts
of BPD.
Therapy, especially
cognitive-behavioral therapy.
The major problems are finding
a qualified therapist and
getting the BPD into therapy.
Researcher Marsha Linehan’s
cognitive-behavioral method of
treatment, called Dialectical
Behavior Therapy (DBT), has
been shown in empirical
research to help BPD patients
experience less anger, less
self-mutilation, and fewer
inpatient psychiatric stays
than patients who received
other forms of treatment.
Other newer and effective
treatments are below as well.
New
Treatment:
MOTR
Effective
Therapy makes a
difference reducing
the severity of BPD
What Works in
Therapy
"DBT IS A
LIFE ENHANCEMENT PROGRAM, NOT A
SUICIDE PREVENTION
PROGRAM." MML
Dialectical Behavior Therapy
(DBT)
Dialectical
behavior therapy (DBT) utilizes the
concept of mindfulness, or being aware
of and attentive to the current
situation and moods, and teaches skills
to control and change intense emotions,
reduce self-destructive behaviors, and
improve relationships.
Read more: Borderline
Personality Disorder: 'Neglected' Mental
Health Condition
Everything
you need to know about DBT and
more
DBT
Skills An
entire page devoted to this topic
DBT's "Half-Smile" video
(younger Borderlines will love
this)
DBT
Self-Help
EXCELLENT SITE!!
Mindfulness Based Cognitive
Therapy (MBCT)
What
is it?
More about
Mindfulness
An in-depth look at
Mindfulness,
MBCT & Thich Nhat Hanh
Transference-Focused
Psychotherapy (TFP)
Treatment associated with
changes in brain activity
Transference-Focused
Psychotherapy
Mentalization-Based Therapy
Mentalization
Based Therapy
Mentalization:
A Patient's Guide
Schema Therapy
(Successful
treatment getting more
recognition)
Schema
combines
elements of CBT and psychotherapy to
refocus the ways people view themselves
and improve self-image, interactions
with others, and cope with problems or
stress.
Schema vs. TFP
What's Your Schema?
Test formulated
by Jeffrey E. Young (on Oprah's
site!)
Schema Therapy
discussed in depth
Systems Training for
Emotional Predictability
& Problem Solving
(STEPPS)
is a type of group
therapy that aims to educate family
members, significant others, and health
care professionals about BPD and gives
them guidance on how to interact
consistently with the person with the
disorder.
About
STEPPS
Article at
website page bottom on
STEPPS.
EMDR
what
is it?
EMDR is a treatment that helps
"reprogram" the brain and
to get at the source of
the trauma that caused the
patient to deal with it,
and whom developed
over-loaded, mis-firing mental
and emotional processes that
became what comprises the
characteristics of a person with
Borderline.
Top
Alternative
Treatments
Blog on
alternative
suggestions
COMBINATIONS OF
TREATMENTS
Successes in treating BPD
|
|
|
This
Page is for ALL Who are in
Relationships with a
Borderline....this page can help you
SAVE YOURSELF.
|
|
|
For
Non-BPD's
An
entire page for you*
 This
entire page has been exclusively
devoted to the persons who
deal directly with a
Borderline, both
personally, in business, in
public, at their job, or
anywhere else that you deal with
people on a close basis.
This
entire page has been exclusively
devoted to the persons who
deal directly with a
Borderline, both
personally, in business, in
public, at their job, or
anywhere else that you deal with
people on a close basis.
*Click
the following link: Where can you
get help?
Top
|
|
|
|
 |
|
|

"Minds
on the Edge"

~ A great book of introduction
|
|
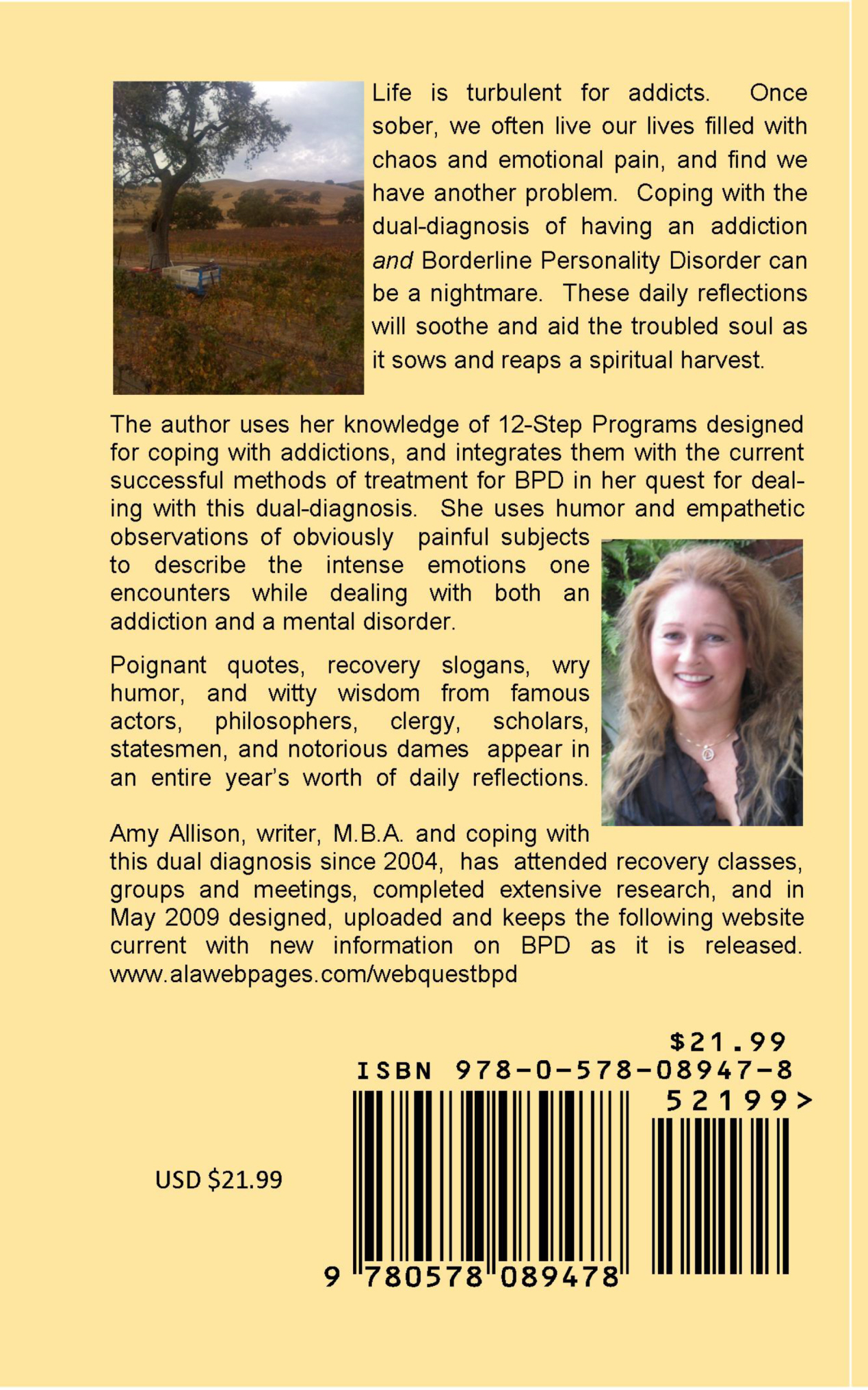
Books
"Destiny
of Detours"
by Amy L. Allison,
website author.
"Prepare
for the Harvest"
by Amy L. Allison, website author.
 |
 |
She is
also the author of
this website. Newly
released in hard-copy on
Lulu Press
website,
and in ebook
format on Smashwords.
A 366-day meditation book
for those with addictions
AND BPD. A universal
link to purchase is also at:
http://www.books2read.com/u/3JGAle.
|
Stronger Than BPD
by
Debbie Corso
Remnants of a Life on Paper
by Pamela and
Bea Tusiani
Beyond Borderline: True
Stories of Recovery
by Perry D. Hoffman and John G.
Gunderson
Girl in Need of a
Tourniquet
by Merri Lisa
Johnson
The Buddha and The
Borderline
by
Kiera Van Gelder
Healing the Child
Within
(go to link
on the left, then at the website, click
on the book's cover for some sample
reading of this
excellent
book)
by
Charles L. Whitfield M.D.
This book
has been in print since 1987. It
is (from cover of book) "A
Discovery and Recovery for Adult
Children of Dysfunctional Families".
Borderlines usually come from
invalidating environments when they were
growing up.
This
poem
sums up the feelings of the
Child Within, and and are often the
emotions of Borderlines. The poem
is also in this book, Chapter 3.
Understanding and Loving a Person with
BPD
by Stephen
Afterburn MD
and Robert Wise
PhD
Loving Someone with Borderline Personality
Disorder by
Shari Y. Manning, PhD.
"Negotiating
With Borderline Personality"
by
Thomas Mengert
Free eBook: Borderline
Personality Disorder: Breaking
the Cycle of Suffering by the Meehl
Foundation.
"The
Essential Family Guide to
Borderline Personality Disorder"
by
Randi Kreger New
tools and techniques to stop
walking on eggshells in dealing
with someone with BPD. (She also
co-authored "Stop Walking on
Eggshells") see below.
"Radical
Acceptance"
by Tara Brach, PhD. Written in 2003,
the book stresses the importance of
incorporating Buddhist mindfulness
meditation in our daily lives.
This is of paramount importance to
the BPD.
"One
Way Ticket to Kansas" by Ozzie Tinman.
See the page
for the Non-BPD's, for
more explanation about all the
references to "The Wizard of Oz" and
BPD.
"Get
Me Out of Here"
by Rachel Reiland
This book was touted by a non-BPD as
being an excellent book by a
recovering Borderline. It
tells the journey of a Borderline's
recovery. An excellent book,
so I am told. One of the best
written by a Borderline.
(More books on page for Non-BPD's,
on the page on Melody
Beattie, and found throughout
site)
"Minds
on the Edge"
by John
Cloud A discussion of
Borderline was featured in an
article in TIME magazine dated
January 19, 2009 in an article
by the same title "Minds on the
Edge". Click the link to
take you to this article.
It has been emailed as a
recommendation to get this into
stock. This book can be
purchased at bookstores or on
Amazon.
"Stop
Walking on Eggshells"
by Paul Mason & Randi Kreger
"Stop Walking On Eggshells Workbook" by Randi
Kreger
"The
Essential Family Guide to
Borderline Personality
Disorder"
by Randi Kreger New
Tools & Techniques to Stop
Walking on Eggshells
"I
Hate You Don't Leave Me"
by
Jerold J. Kreisman is a great
starting point for those who
want to better understand BPD.
It was one of the first books
written for the lay person. It
assumes a very low existing
baseline of knowledge, without
patronizing the reader.
"The
Handbook of
Mentalization"
by Jon G.
Allen/Peter Fonagy
"What
Works for Whom?"
by Peter
Fonagy
(entire book online!)
For more books for BPD's AND
Non-BPD's, go to this link.
|
|
Top |
|
|
|
Stig-ma:
a symbol of disgrace or infamy.
|
|
|
|
|
|
|
Site Created by
Odyssey
Design
Copyright © 2009-2025
Odyssey Design
-- All Rights Reserved
|
|
|
|
|
Blogs
About BPD
New York Times
BPD
blog
Anonymous Blog of
a real-life Borderline
as
it happens
I have
gotten permission to
follow a BPD's Journey
of Recovery in a personal
blog on Blogger.com.

Top |
|
For
the Professionals
For
the Professionals
For
the
Professionals
For
the
Professionals
[Success
in Recovery]
NEW YORK (Reuters
Health) - For those
suffering from
borderline personality
disorder, friends and a
job may be harder to
secure than symptom
relief, according to a
new study.
"There's been this idea
that if people had fewer
symptoms of the
disorder, then they
would naturally evolve
socially and
vocationally," lead
researcher Mary Zanarini
of McLean Hospital in
Belmont, Massachusetts
told Reuters Health.
"That does not seem to
be true."
So Zanarini and her
colleagues followed 290
people with borderline
personality disorder, 93
percent of the patients
had at least one 2-year
break from the symptoms
of the disorder during
the 10 years, and 86
percent had at least one
4-year symptom-free
period. Once achieved,
symptoms rarely
returned.
However, only about 50
percent of patients
achieved full recovery,
which was defined as a
reprieve from symptoms
lasting at least 2
years, plus good social
and vocational
functioning. Of those
that did reach this
mark, about a third
later redeveloped
symptoms, or once again
struggled socially or
with their job.
By Lynne Peeples
Top
|
|
A short page
has been directed at those
therapists
who have not been trained
in Borderline treatments, or
currently do not handle
Borderlines in their
caseload.
Please go to the link above for
this page.
The
discussions
below touch on
pertinent topics (in the way
of linked-to information), and
is hopefully helpful,
nonetheless.
FOR PROFESSIONALS
The
Journal
of the California Alliance
for the Mentally Ill
This is an 84-page document
published by the above
organization. Be
sure to set the "viewing %" at
100% for easier reading, both
while on your computer screen,
or if you should print it
out. It can
be printed for you use
distribution to clients or
other interested
persons. This is not a
recent article, but highly
informative. Below are
findings for various
components of BPD.
Top
--- End of Section---
|
|
A Matter of Personality
- From
borderline to narcissism
by David M. Allen, M.D.
Why
Does the Predominant
Treatment Paradigm for
Borderline Personality
Disorder Neglect Family
Dynamics? What is
invalidation and what role
does it play? Published on
February 11, 2012 by David
M. Allen, M.D. in "A Matter
of Personality".
Marsha
Linehan is the creator of
what is currently the most
prominent psychotherapy
paradigm used to treat
Borderline Personality
Disorder (BPD). Her
Dialectical Behavior
Therapy (DBT) is often
said to be the most
"empirically-validated" of
all such psychotherapy
treatments. Actually, DBT is
only "empirically validated"
mostly for the treatment of
one symptom of BPD called
parasuicidality. But I
digress.
Dr.
Linehan's theory of the
cause of BPD, for which she
cited no actual scientific
evidence when she first
described it (although there
has been some since), is
called the "biosocial
model." BPD, she
believes, is created
primarily by two
factors. The first
is the patient's
genetic tendency to become
emotionally dysregulated.
Individuals with the
disorder are highly
reactive. They respond
quickly and very strongly to
environmental events and are
slow to recover from this
"dysregulated" state.
Whether
the tendency towards
becoming emotionally
dysregulated is something
purely genetic in origin or
is the result of
environmental factors in
genetically-vulnerable
individuals is an open
question. Clearly both
genes and environment
contribute to most
personality traits, but how
much of each is
required? I will
mention some evidence for
the answer to this question
later in this post.
The
second causal factor in the
genesis of BPD, according to
Linehan, is what she refers
to as an invalidating
environment.
Invalidation,
as used in psychology, is
not merely people
disagreeing with something
that another person said. It
is rather a process in which
individuals communicate to
another person that the
opinions and emotions of
that person are meaningless,
irrational, selfish,
uncaring, stupid, most
likely insane, and wrong,
wrong, wrong.
Invalidators
let it be known directly or
indirectly that their
target's views and feelings
do not count for anything to
anybody at any time or in
any way. In some families,
the invalidation becomes
extreme, leading to physical
abuse and even murder.
However, invalidation can
also be accomplished by
verbal manipulations that
invalidate in ways both
subtle and confusing.
Dr.
Linehan wrote only briefly
in her book
(Cognitive-Behavioral
Treatment of Borderline
Personality Disorder) about
which environment she is
talking about as being
invalidating (page 56-59),
and she barely mentions it
in her talks and
videos. It is the
family environment in which
the person grew up.
Really, what else could it
be? Of course, your
spouse and friends can also
invalidate you, but why
would you choose to fall in
with an unpleasant group
like that if you were not
already accustomed to this
sort of treatment?
When
it comes to DBT, however,
most of the energy in the
psychotherapy treatment
described by Dr. Linehan is
directed at helping the
patients accept themselves
as they are, without much
said about how they got that
way in the first place,
combined with teaching
patients other skills that
are helpful in reducing
their emotional
reactivity. These are
referred to sometimes as
self-soothing skills, and
are presumed by many DBT
therapists to be something
that patients with the
disorder just never
learned.
I
sometimes give my patients
with BPD handouts which
describe these skills from
Dr. Linehan's Skills
Training Manual. I
usually find that patients
have already tried at least
some of these techniques on
themselves without having
had any instruction at
all. That makes me
wonder if perhaps their
apparent lack of knowledge
about the techniques in some
interpersonal environments
actually reflects a strong,
fear-induced desire not to
use such skills, rather than
an actual absence of
them.
In
her book, Dr. Linehan does
say that she focuses on the
patient's interpersonal
skills later in the therapy
process. She even
mentions that family therapy
might be included.
Mentions it once or
twice. The first time
on page 420 of her
book. She does
not say anything about what
that family therapy might
entail.
If an invalidating
environment is one of two
main causes of the disorder
as she theorizes, how come
she does not address this
very much in her treatment
plan?
A
few months ago, a story in
the New York Times about Dr.
Linehan possibly shed some
light on this
question. Dr. Linehan
admits that when she was
younger, she "attacked
herself habitually, burning
her wrists with cigarettes,
slashing her arms, her legs,
her midsection, using any
sharp object she could get
her hands on." She added, "I
felt totally empty, like the
Tin Man." Self
injurious behavior and
feeling empty are two of the
hallmark symptoms of
BPD. Did she have the
disorder? According to
the article at least, BPD is
a diagnosis "that she would
have given her young
self."
I
have only personally met Dr.
Linehan once very briefly,
and she was perfectly
appropriate and
personable. However, I
had heard the occasional
rumor from other researchers
that she has a little bit of
the BPD in her.
So
why has she so studiously
avoided family dynamics in
her treatment paradigm when
an "invalidating
environment" is fully half
of her theory about the
cause of borderline
personality
disorder? And
why would she include an
invalidating environment in
her theory if she, as
someone who has struggled
with the disorder, had not
been invalidated
herself? If her theory
is true, she of all people
would have experienced
that.
The
Times article does describe
her family a bit, but there
does not seem to be a whole
lot of dysfunction in the
description:
"Her childhood, in Tulsa,
Okla., provided few clues. An
excellent student from early
on, a natural on the piano,
she was the third of six
children of an oilman and his
wife, an outgoing woman who
juggled child care with the
Junior League and Tulsa social
events. People who knew the
Linehans at that time remember
that their precocious third
child was often in trouble at
home, and Dr. Linehan recalls
feeling deeply inadequate
compared with her attractive
and accomplished siblings. But
whatever currents of distress
ran under the surface, no one
took much notice until she was
bedridden with headaches in
her senior year of high
school. Her younger
sister, Aline Haynes, said:
"This was Tulsa in the 1960s,
and I don't think my parents
had any idea what to do with
Marsha. No one really knew
what mental illness was."
This
description makes it sound
as if she were just mentally
ill for some unknown reason,
and that that was the whole
explanation for her
behavior, does it not?
She just somehow acquired a
messed up brain. But
that would only be half of
her DBT theory, and a
problematic part of the
theory at that.
In
one study by researcher
extraordinaire Andrew Chanen
and others, adolescents who
presented for the very first
time with BPD did not show
the volume reductions
previously observed in parts
of the brain's limbic system
in many samples of adults
with BPD (the hippocampus
and amygdala) - two of
the MRI findings of adult
BPD brains considered to be
the most significant. They
did, however, show small
changes in one other part of
the brain compared to
controls. (Psychiatry
Research: Neuroimaging 163
[2008] 116-125).
This
finding could mean that some
of the brain phenomena that
may create high emotional
reactivity arise primarily
from the effects of some
other factor or
factors. An effect,
not a first cause. What
factors might they be?
An environmental
factor? I would
suspect so. Perhaps
the invalidating
environment?
So,
again, why does Dr. Linehan
relegate changing family
behavior to what is
basically a footnote in her
treatment text? Of
course I have no way of
knowing the answer to this
question in her case.
With
my patients who do not want
to look too closely at their
family dynamics, however,
the reason why is crystal
clear. They are very
protective of their
families, even if they
complain unceasingly about
them. They really do
not want anyone to think
badly of their family
members, so they tend to
keep the skeletons in the
family closet to themselves,
at least at first.
(In
cases where they do try to
make their family members
look bad, as some patients
with BPD do, they often do
so in a way which makes the
listener doubt their
truthfulness or their
ability to remember things
correctly. In other
words, they do so in a way
in which they invalidate
themselves).
Maybe
if you just ignore a big and
recurring family problem, it
will go away. Not.
Top
Mentalization-Based
Treatment – a Patient’s
Guide (MBT)
What is
MBT?
MBT is a
type of psychotherapy
created to treat people
with borderline
personality disorder. It’s
also been found to be
useful for people with
other types of mental
illness. As the name
suggests, it centres on
the concept of
‘mentalization’. I
struggled to understand
what exactly this is,
which could be further
evidence of my need for
this therapy or just that
I’m a bit dim. But I
finally grasped that it’s
very straightforward.
Mentalization is simply
about recognising what’s
going on in our own heads
and what might be going on
in other people’s heads.
So what’s the big deal?
Surely we’re all pretty in
touch with what we’re
thinking and feeling, and
have got as good a chance
as anyone else of guessing
what others are doing? Er,
no. Unfortunately those of
us with BPD are unlikely
to be top scorers in the
Minds’ Awareness League.
Not great at accurately
identifying what’s
happening in our own minds
and even less likely to
correctly work out what’s
in other people’s minds.
Especially if we’re
feeling stressed out.
And there’s an even more
fundamental problem here.
When we’re feeling crap,
we’re likely to shut down
(or at best tone down) our
ability to ‘mentalise’.
Thinking becomes a real
effort, and reasoned
thinking about thinking
nearly impossible.
Certainly for me, when
things are tough I often
self-harm specifically to
avoid thinking, as that’s
too painful. Self-harming
gives us something very
concrete to focus on,
which links with another
aspect of BPD. Apparently,
if we’ve got BPD we tend
to find it easier to
believe things that we can
see rather than imagining
what might have led to a
particular situation. (No
money under the pillow,
definitely no tooth
fairy.)
MBT is intended both to
help us sharpen up our
ability to mentalise and
to be willing to use it,
especially when we’re
feeling intense emotions.
For example, in a session
the therapist might ask us
to consider what the other
person in a difficult
situation might have been
thinking, and help us move
past our initial
assumption, especially if
it’s a really negative
one.
Top
What’s the
difference between
‘mentalising’ and
thinking, and why can
mentalising sometimes be
better?
Thinking is thinking.
Mentalising is thinking
about thinking and
feeling, our own and other
people’s. Obviously it’s
often best just to get on
and have thoughts. About
whether Borat is
the funniest film ever
made or a shocking and
trashy piece of sexist and
racist rubbish. About
whether there’s something
we can do as a
non-punitive alternative
to self-harming.
I’ve found
it helpful looking at
mentalising from the
perspective of people with
autism. Perhaps it’s
because I’ve struggled to
understand quite what
mentalisation is about
that it’s been useful to
me to consider a group of
people with a totally
different disability to
mine. People with autism
live very much in the here
and now. They have been
described as having no
‘theory of mind’, as most
are unaware of their own
thinking processes and
have even less recognition
that other people think or
have feelings. Clearly
people with autism think.
(An inordinate amount of
the time, it seems, about
Thomas the Tank Engine, at
least when they’re kids.)
But it’s a very automatic
experience, and reflecting
on their own thoughts just
doesn’t arise. And the way
they see the world is such
that although they may
notice the manifestation
of others’ thoughts and
feelings, for example they
can see that someone is
smiling or hear them
shouting, they don’t
connect that with the
emotions that produce
those observable
responses. People with
autism find it almost
impossible to imagine
themselves ‘in someone
else’s shoes’.
For those of us with BPD
rather than autism,
mentalising is an
acquirable skill, and one
which can give us valuable
extra perspective on a
situation. For example, if
I’m planning to take an
overdose, just thinking
about it tends to take me
along a route which lets
me confirm this is the
‘right’ thing to do. But
if I have to mentalise, I
have to look at my
thinking. It’s hard for me
to do this without
concluding that I’m not
thinking straight. That my
thoughts and feelings
about the overdose are
caused by feeling
seriously crap and that I
should at least try to
hold off any decision til
I’m feeling more settled.
And if I
then move on to thinking
about others’ thoughts
and feelings, it takes
me to the painful place
of knowing how
traumatised my friends
are if they find out
that I’ve taken an
overdose. Let alone the
impact on them if the
next overdose turns out
to be fatal.
None of this mentalising
necessarily stops me
from taking
self-damaging action but
it at least gives my
self-protective side a
decent shot at
introducing some logic
to the situation.
Top
What’s It
Like Having MBT?
You might expect that a
therapy with mentalisation
at its heart would involve
the therapist endlessly
asking “And what was in
your mind? And what was in
their mind?” But, luckily,
this hasn’t happened. It’s
all much more nuanced than
that. Similarly, although
the approach is very
non-directive, when I ask
for advice or need help in
practical problem-solving
with something I’m
wrestling with, my
psychiatrist will often
respond in a ‘normal’ way
and help me out.
I had
cognitive behavioural
therapy with a
psychologist before I
ended up being
sectioned. At that
stage, I was taken on by
a personality disorder
unit as an outpatient
and have had MBT weekly
with a psychiatrist for
about 18 months. Both
types of therapy feel
very similar, despite
the psychologist and
psychiatrist being very
different types of
people. Both approaches
have felt supportive,
non-judgmental and
focused on what I’m
thinking. I’ve been able
to see issues,
especially painful ones,
from a different
perspective and to
understand what might be
fuelling the tough
stuff. Both have made me
feel like I’m setting
the agenda about what we
talk about and that I
can say anything,
however embarrassing or
ridiculous I feel it is.
And I know that the
self-protective part of
me, which tries to
resist my
self-destructive
tendencies, gets crucial
reinforcement.
The most
noticeable difference in
style is that my
psychiatrist has very
‘high boundaries’, so I
know almost nothing
about him and his life,
other than what I can
pick up from clues
around his office. (He
either rides a motorbike
or is excessively
worried about getting a
head injury when driving
his car.)
Perhaps
the most tangible
difference I experience
is that I’ve only once
self-harmed after a
session with the
psychiatrist whereas I
used to do so regularly
after my previous
sessions. This really
puzzled me til I read a
couple of books about
MBT. These made me
realise that while the
MBT sessions feel quite
normal and
‘spontaneous’, they’re
carefully designed to be
at a level of intensity,
or intrusiveness, that I
can comfortably cope
with. (This relates back
to the business about us
closing off if things
become too painful.)
This doesn’t mean that
I’m never moved outside
my comfort zone – most
sessions we cover things
which make me cry. But
somehow, overall I don’t
end up feeling
completely jangled or
bursting with feelings I
don’t know how to or
don’t want to deal with.
Top
Does
It Work?
Well,
I’ve been able to
survive 18 months of
pretty consistent
suicidal feelings and
still be around to
write this. And
studies have shown
that it certainly
works for a lot of,
but not all, patients.
One very reassuring
thing is that it’s
been designed as a
result of careful
research into both the
causes of BPD and the
impact of MBT. I don’t
really understand all
the stuff about how
BPD develops, but it
goes something like
this.
If
mothers have problems
connecting well with
their babies, they
respond differently to
other mothers. One
thing that the
research shows is that
when the babies are
really upset, these
mothers don’t calm the
babies in a way that
helps the babies to
‘understand’ or learn
what’s their own
distress and what’s
the mother’s. It’s a
bit like the baby’s
distress is magnified
and bounced back at
the little thing
rather than being
soothed and dissolved
by the mother. As well
as emotional mishaps
like this, it’s been
found that many people
who develop BPD often
have early experiences
of abuse or neglect by
parents. These things
lead to many of us
being unable to soothe
ourselves in ways that
are conventional, or
not self-destructive,
again reinforcing our
tendencies to
self-harm.
Another
central proposition of
MBT is that when we’re
babies and our mothers
aren’t able to comfort
us in an effective
way, we sort of bung
onto our mother the
parts of ourselves we
can’t cope with. This
results later on in
life with us coping
particularly badly
with the loss of
someone close to us,
partly because we
might have ‘assigned
over’ to them the
painful parts of
ourselves. This
contributes in a
rather complicated way
to our tendencies to
self-harm and be
suicidal, apparently
to feel re-connected
to the outsourced part
of ourselves.
The
quality of
‘attachment’ in our
earliest years
continues to affect
how we feel and think
right through our
lives, and if they’ve
got off to a bad start
we’ll have
difficulties with
other close
relationships.
Including potentially
the one with our
therapist.
The MBT
therapist, then, will
be very aware of this
and will be careful
that we don’t just
slot back into a
pattern of feeling
overwhelmed by
intensely painful
feelings which make us
close off thinking,
especially about our
own and the
therapist’s thoughts.
Feeling understood by
someone we trust (the
therapist), is a sound
place to be able to
move into a calmer,
safer way of coping
with difficult stuff.
|
|
| |
Recent Research Findings
New evidence
and a study of 5,496 twins in
the Netherlands, Belgium and
Australia drew the conclusion
that 42 percent of variation
in BPD features was
attributable to genetic
influences and 58 percent was
attributable to environmental
influences. There is
more of a link to genetics of
the disorder than previously
thought.
Although the cause of BPD is
unknown, both environmental
and genetic factors are
thought to play a role in
predisposing patients to BPD
symptoms and traits. Studies
show that many, but not all,
individuals with BPD report a
history of abuse, neglect, or
separation as young children.
Forty to 71% of BPD patients
report having been sexually
abused, usually by a
non-caregiver. Researchers
believe that BPD results from
a combination of individual
vulnerability to environmental
stress, neglect or abuse as
young children, and a series
of events that trigger the
onset of the disorder as young
adults. Adults with BPD are
also considerably more likely
to be the victim of violence,
including
rape and other
crimes. This may result from
both harmful environments as
well as impulsivity and poor
judgment in choosing partners
and lifestyles.
NIMH-funded
neuroscience research is
revealing brain mechanisms
underlying the impulsivity,
mood instability, aggression,
anger, and negative emotion
seen in BPD. Studies suggest
that people predisposed to
impulsive aggression have
impaired regulation of the
neural circuits that modulate
emotion. The amygdala, a small
almond-shaped structure deep
inside the brain, is an
important component of the
circuit that regulates
negative emotion. In response
to signals from other brain
centers indicating a perceived
threat, it marshals fear and
arousal. This might be more
pronounced under the influence
of drugs like alcohol or
stress. Areas in the front of
the brain (pre-frontal area)
act to dampen the activity of
this circuit. Recent
brain-imaging studies show
that individual differences in
the ability to activate
regions of the prefrontal
cerebral cortex thought to be
involved in inhibitory
activity predict the ability
to suppress negative emotion.
Serotonin, norepinephrine and
acetylcholine are among the
chemical messengers in these
circuits that play a role in
the regulation of emotions,
including sadness, anger,
anxiety, and irritability.
Drugs that enhance brain
serotonin function may improve
emotional symptoms in BPD.
Likewise, mood-stabilizing
drugs that are known to
enhance the activity of GABA,
the brain's major inhibitory
neurotransmitter, may help
people who experience BPD-like
mood swings.
Back to General
Information
Top
Holidays or any major
interruption to a
Borderline's daily patterns
can be disruptive and
disconcerting.
Stress and the Borderline
|
|
|
|
Does
BPD Have a Spiritual
Solution?
by
Clive
Green
Borderline Personality
Disorder is a mental disorder
that requires the adjustment
of individuals and their loved
ones. It requires that their
loved ones learn how to avoid
them when in hyper-hysteric
fits and it requires that the
individuals with the disorder
learn to avoid their family
when they are tempted to do
them emotional harm. In time,
the solution of problem
avoidance isn't enough,
however. Inevitably the
sufferers need to tell someone
of how badly they wish they
could die or destroy everyone
who doesn't totally adore
them.
These kind of
hysterics are not a matter of
mere drama or pretense, they
demand to be expressed and if
the sufferers fail to express
them they are sure that they
will just die. Of course, the
reality is much different than
the illusion that these
individuals create in their
mind. The reality is that the
people suffering from BPD have
disconnected with their wise
mind, their real mind.
They have gotten
to a point where they have a
hard time believing there is
anything to the world around
them except what their
intellectual mind or their
emotional mind tells them
there is. The reality is that
when they get stuck into one
of these modes of thought as
is true most of the time, they
will either turn their friends
off with manic attempts to
share every bit of
intellectual information that
they find interesting. This
will send the friends away
because it is just too boring
for the friend to endure. The
other tactic that the BPDs
will use is to share whatever
they are feeling at the
precise intensity that they
are feeling it.
This usually
frightens friends or family
away unless they have learned
to deal with it. The case of
the BPD sufferer is that they
are damned if they do and
damned if they don't. So, as
the cruelty of this disorder
is made clear the ethical mind
is challenged to ask, how
could this be? How could God
allow this suffering? Of
course, God has little to do
with it. God, in fact is the
one who is able to heal the
entire illusion, because
especially with this type of
suffering, illusion is the
best word to describe what it
is. The pains and frustrations
that lead the sufferer to push
into one of these extremes
(emotion or intellectualism)
is the same dysfunction that
everyone experiences in the
ego-bound mind except it is
magnified for the BPD
sufferer.
The result is
contrary to what might appear
obvious that the BPD has an
easier time releasing ego and
accepting God. So, the
question is there a spiritual
solution to BPD, is somewhat
misleading. Perhaps a better
question would be, what is BPD
a spiritual solution for? The
answer to that of course is
that BPD is the spiritual
solution for the illusion of
ego-bound time. It is a
guidance system in the same
way that the two buffers of a
bowling alley is a guidance
system. They teach the BPD to
shoot at the middle and avoid
the comfortable edges.
The middle where
intellect and emotion meld
into a powerful unit is the
perfect place for all who live
in this time-bound reality,
because this middle area
teaches the soul that it is
always connected to well-being
while always being connected
to the illusion of time and
space. The spiritual truth of
this reality is that we are
all paradoxes walking around
as if we aren't paradoxes. The
existence of this paradox is
something that constantly
pushes people into either
psychosis or more commonly,
neuroses. The BPD sufferer is
never able to get lost in the
apparently comfortable world
of neurosis and is also never
able to flee into the secure
insecurity of psychosis.
Rather, they
are constantly tied to the
pain of the borderline, until
they free themselves from ego
- the one source of their
apparent suffering. There are
therapies available that can
help the individual to develop
their mindfulness and release
the disabling aspects of BPD.
Back
to Problems
|
|
The Etiology
of BPD
by
A.J. Mahari
I
will be outlining the
etiology of BPD - its
causes. I know that no one
has the definitive answer
about exactly what one thing
or combination of things
makes up the root causes of
BPD. I, do, however, based
upon my own experience, have
some fairly strong feelings
about this.
Many
put forth that the causes of
BPD are still not well
understood, and it is likely
that a number of factors are
involved in its development.
I can partially agree with
that. It is the causative
factors of anything that
may, in fact, be biological
that I have difficulty with
along with the amount of
medication being thrust upon
borderlines.
One
biological theory purports
that traumatic experiences
in early childhood may cause
the hippocampus to atrophy
which is thought to cause
structural brain changes in
individuals with BPD. I
don't know. I would say
though that isn't it just as
likely that the effects of
trauma on the brain that can
cause changes in brain
development are the result
of the early childhood
emotional and psychological
trauma and not some genetic
mutation in those with BPD.
Further to this, I've had
many professionals I've
asked tell me that they
believe that traditional
psychotherapy can positively
impact trauma-induced
changes in the brain and
build lasting changes that
can address any such damage
-- so why the big push with
medication?
I
think what needs to be
focused on most is that
there are likely a number of
factors rather than coming
down so strong on the side
of the biological argument.
I've
had BPD and recovered from
it. I had some neurological
testing done when I was
borderline and I don't have
any atrophy or any such
process in the hippocampus
of my brain. That is not to
say that some haven’t
obviously had that result
but is that really what
causes BPD or is it a
coincidence? I wonder.
It
is further theorized by many
that this dysfunction in the
limbic system of the brain
may explain some of the
emotional dysregulation
which is inherent in BPD.
That may well be, but, do we
need medication to control
that or can we learn new
ways of thinking and
believing that re-route the
neurons in our brains and
make the necessary
adjustments or changes
needed to recover?
I
would assert that how one
thinks and what causes the
cognitive distortions and
polarized way of thinking in
those with BPD is far more
responsible for emotional
dysregulation then some
physical problem in one's
brain. I believe most BPD
responses to stress and to
relational difficulties have
their main genesis in the
core wound of abandonment.
I
have written a 253 page
ebook called, "The Legacy of
Abandonment in BPD" - An
examination of the core
wound of abandonment and
Borderline Personality
Disorder that is a follow up
to my first ebook, "The
Abandoned Pain of Borderline
Personality Disorder" which
is a detailed history, from
the inside out, as someone
who has been there and
recovered from BPD, of how
and why the abandoned pain
of those with BPD keeps them
stuck in the agonizing and
seemingly mystifying
suffering of Borderline
Personality Disorder. This ebook is also a precursor to
the ebook that followed it,
"The Shadows and Echoes of
Self - The False Self That
Arises Out of the Core Wound
of Abandonment". In BPD Each ebook is available
separately or all 3 can be
purchased together with or
without audio programs as
well. The core wound of
abandonment is traumatic
enough to perhaps cause some
changes on a biological
level. What I take issue
with though as the
biological theories are put
forth is that there are not
contained in those theories,
or articles, the reality
that many are recovering
from BPD and that DBT Skills
Training Schema Therapy and
Cognitive Behavioral Therapy
along with psychotherapy -
talk therapy - can and will
(in most cases) address the
organization of thoughts
based upon reactionary
protective instinctual
behavior while under the
stress of the trauma to the
point where one can change
the way they think and more
or less reverse the damage
and/or manage their way out
of BPD.
© A.J. Mahari 2006
Top
|
|
The
Use of Dialectical Behavior
Therapy in a Small Community
Health Setting
by Leah Jaquith,
Ph.D., Washington County
Community Mental Health Services
Washington County
Community Mental Health Services
is a small (1,400 client)
full-service community mental
health center located in rural
Ohio. Washington County is one of
a handful of single MHAR boards in
the state. We have never been
successful in getting a mental
health levy passed and thus always
struggle to provide maximum
service for minimum dollars.
As our agency was
developing programming to meet the
needs of the community we began
implementing treatment for
individuals diagnosed with
borderline personality disorder
based on Marsha Linehan’s
Dialectical Behavior Therapy
model. One of the reasons I was
interested in the DBT model was
because I had seen it used so
successfully in community mental
health in New Hampshire and
because its principles were so
consistent with those of the
Recovery Model promoted by the
Ohio Department of Mental Health.
DBT, like Recovery, places the
emphasis on the individual being
allowed to take responsibility for
the direction of their mental
health treatment and for
decision-making in their lives.
DBT is an amalgam of
cognitive-behavior therapy which
includes a variety of coping
skills, validation of the
individual’s emotional experience
and coaching to help the
individual make choices that are
adaptive rather than
self-destructive or
self-defeating.
DBT assumes that
individuals with borderline
personality disorder have in
common an inability to effectively
regulate their emotions. This high
sensitivity to negative emotional
stimuli and an intense response to
such feelings often leads to
attempts to escape the negative
emotions that are maladaptive.
Such responses share the
characteristic of their
representing an often-desperate
attempt to escape the negative
emotional state. Substance abuse,
self-mutilation, overeating,
engaging in risky behaviors such
as sexual encounters, stealing,
speeding in cars and making
suicidal gestures are all common
responses to the negative
emotional experience. And while
these activities can provide
immediate distraction or relief,
overall they solve nothing and
often leave the individual with
more difficulty than before they
engaged in these escaping
behaviors.
DBT represents an
attempt to offer individuals with
the diagnosis of borderline
personality disorder the
opportunity to learn new ways to
tolerate emotional pain, make
decisions that lead to productive,
problem-solving activity and to
receive validation for the
emotional pain that has driven the
maladaptive behaviors. In essence
we offer the opportunity to
substitute the non-productive
behavior with an understanding of
triggers for their behavior and a
repertoire of productive
alternatives.
The structure of DBT
at our clinic is dictated to some
degree by our size and financial
limitations. We run two
introduction-to-DBT concepts
groups per week for women. We have
three DBT groups that familiarize
women with the DBT concepts and
skills of mindfulness, emotion
regulation, distress tolerance and
interpersonal effectiveness. These
groups meet for two hours each
week. In addition, all group
members must have individual
therapy that is based on DBT
principles. DBT group members are
encouraged to practice and
document the success or problems
they encounter in using their
skills in their day-to-day lives.
They are supported in their
emotional expression of distress
but often confronted, sometimes in
an ironic or humorous manner,
about their tendency to
catastrophize. They are encouraged
to think of skills to use to help
them tolerate the emotional
distress. When DBT group members
make a suicidal threat or gesture
(called parasuicidal gestures by
Linehan), individuals are
frequently not hospitalized after
they are declared medically
stable. Instead, they are reminded
of the principles of DBT, which
suggest that learning to tolerate
the discomfort is key in
developing more adaptive responses
to stress and to their recovery.
In group, they are free to
question techniques or skills,
describe skills they used or had
difficulty with and work on skills
sheets that offer new concepts or
skills. Larger agencies often have
distinct DBT teams who do only DBT
with a certain group of clients.
In our small agency we do DBT as a
part of the other work we do.
However, we are committed to the
concepts and make sure that the
availability for coaching is
honored. I believe that it is
essential to remove the need for
these women to do something
“dramatic” to get attention. Quite
the contrary, we want to support
their desire to learn and we make
coaching an easy and routine thing
for them to request and receive.
Easy access to
support, clear and well-maintained
boundaries and lots of
encouragement and information
about feelings are all aspects of
DBT that make it successful in
helping women with emotional
dysregulation challenges. All
women in the DBT groups are able
to make phone calls during the day
and up to 9 P.M. in the evening
(through the crisis line) to their
group facilitator or their DBT
individual therapist. The phone
calls have constraints: no
discussion of suicidal plans or
activity. The call focuses on the
coaching aspect of the DBT program
where the individual is helped to
understand what she is feeling,
what may have triggered these
feelings and a review of skills
that the individual has indicated
have been helpful to relieve these
feelings in the past.
Our success with DBT
programming has led us to expand
and we now have a DBT group for
men and are in the process of
developing one for teenage girls
with emotion regulation
challenges. We have partnered with
the local developmental
disabilities board and their
contract providers to adapt DBT
principles for dually diagnosed
individuals (DD/MH) we share. This
partnership has been generally
successful and has led to our
providing trainings to DD staff
regarding the use of coping skills
with other DBT clients and in
fostering more adaptive responses
in our shared clients.
We are fortunate in
that the hospitals with whom we
work (Appalachian Behavioral
Healthcare and Marietta Memorial
Hospital) have been open to
learning about DBT and DBT
interventions. In order for
clients who typically have been
admitted to the hospital to learn
to tolerate some emotional
discomfort and to be encouraged to
use skills to do so, they cannot
continually be admitted to
psychiatric hospitals. The DBT
model suggests that if an
individual has made a parasuicidal
gesture (e.g., scratched wrists,
taken pills) that they be
medically stabilized and returned
to the community with appropriate
supports (crisis appointment, case
management, coaching in skills,
attempt to follow the “chain” that
led to their emotional upset). As
you might imagine, this feels
quite risky to emergency room
personnel and those unfamiliar
with DBT principles. However, the
psychiatrists at both hospitals
have been supportive of our
interventions and have helped pave
the way for us to work closely
with emergency room personnel in
this area as well.
Overall, the
implementation of DBT programming
and the institutionalization of
DBT principles has led to a
reduction in hospitalization,
parasuicidal gestures and to
reports of increased satisfaction
with their lives in our DBT group
members. The most gratifying
result comes when our DBT members
report that they have successfully
managed a situation that in the
past would have overwhelmed them.
Like any program,
DBT relies on the individual’s
desire to change. This program
requires lots of participation on
the part of our members. The two
greatest challenges we face are
engaging individuals who do not
believe they can or are ready to
change and move toward recovery,
and working with individuals who
are still actively misusing
substances such as alcohol or
street /prescription drugs. As
long as they can numb themselves
or escape with the substance, the
attractiveness of learning skills
to tolerate emotional distress is
diminished.
Back
to DBT
section
Back to
Top
|
|
BORDERLINE
CHARACTERISTICS
(From Marsha Linehan’s book &
internet)
1.
Shifts in mood lasting only a few
hours.
2. Anger that is inappropriate,
intense or uncontrollable.
3. Self-destructive acts:
self-mutilation or suicidal
threats and gestures.
4. Self-damaging impulsive
behaviors are alcohol & drug
abuse, compulsive
spending,
gambling, eating disorders,
shoplifting, reckless driving,
compulsive
sexual behavior, food addiction.
5. Marked, persistent identity
disturbance shown by uncertainty
in at least two
areas:
self-image, sexual
orientation, career choice,
friendships, values.
6. Chronic feelings of emptiness
or boredom.
7. Unstable, chaotic intense
relationships characterized by
splitting.
8. Frantic efforts to avoid real
or imagined abandonment.
9. Stress-related paranoid
ideation or severe dissociative
symptoms.
-
Splitting:
the self and others are viewed
as "all good" or "all bad."
-
Alternating
clinging and distancing
behaviors.
-
Great
difficulty trusting people and
themselves.
-
Sensitivity
to criticism or rejection.
-
Feeling
of "needing" someone else to
survive.
-
Heavy
need for affection and
reassurance.
-
Some
people with BPD may have an
unusually high degree of
interpersonal sensitivity,
insight and empathy.
-
36%
of us will attempt suicide who
meet all 9 criteria of
Borderline.
9% of us will attempt suicide
who meet 5-7 of criteria for
Borderline.
8 out of 100 suicide attempts
of Borderlines are fatal;
higher with dual diagnoses
and/or coupled with other
addictions.
75% of Borderlines are
self-harming (does not include
any of suicide stats).
· Additional
addition issues, usually present
in BPD patients, should be treated
by a therapist versed in
experience in recovery issues,
most notably in the sexual &
food addictions and substance
abuse. Group therapy and
supportive 12-step programs are
available and important tools for
recovery from most addictive
behaviors.
· Substance
abusers (including drugs, porn,
alcoholic, narcotics, food) along
with BPD have a
higher % of suicidal
behaviors than
patients with only BPD (9-35%)
or only substance abuse
(7%)…more like 16-42% or more.
Top
|
|
Statistics
for
Borderline Personality Disorder
!!
IMPORTANT
CHART BELOW !!
A diagram
of BPD, addiction and mental illness
statistics for the U.S.
Substance Abuse & Borderline
Personality Disorder
STATS
& FACTS
Teen
Statistics: 1
in 5 teens lives with a mental
health condition. 50% of
these teens show symptoms by the
age of 14. In other words, 1
in 10 teenagers enters high school
demonstrating symptoms of having a
probable mental illness. NAMI
(The National Alliance on Mental
Illness) goes on to say that there
is a delay of 8-10 years between
the emergence of the symptoms and
intervention to address the
illness. This
is disturbing. NAMI
has 2 programs: "Say It
Out Loud", and "Ending The Silence",
that reach out to teens to enable
them to speak out and seek help
for themselves.
STATS
& FACTS
All
Mental Illness Stats:
Global/General Facts & Numbers
(from NAMI magazine)
1 in
4 adults experiences a mental
health disorder in a given year.
1 in 17 adults lives with a
serious mental illness.
1 in 10 children lives with a
serious mental/emotional disorder.
According to 2004 World Health
Report, major depressive disorder
is the leading cause of disability
in the U.S./Canada between 15-44.
Anxiety disorders frequently
co-0ccur with depression or
addiction disorders.
One half of all lifetime cases of
mental illness begin by age 14,
3/4 by 24.
Adults living with serious mental
illness die 25 years earlier than
other Americans.
Suicide is the 11th leading cause
of death in the U.S.
75% of youth in juvenile justice
systems have at least one mental
disorder.
STATS
& FACTS
The Suicide Rate for
Borderlines is 60 times
that of the general
population.
STATS
& FACTS
from
the New England Journal of
Medicine website
Borderline Personality
Disorder
Posted by Abigail Place
The latest article in our Clinical
Practice series, Borderline
Personality Disorder, reviews the
characteristic features of
borderline personality disorder,
evidence to indicate genetic and
environmental factors in
pathogenesis, and effective
treatment strategies.
BPD
is present in about 6% of primary
care patients and persons in
community-based samples and in 15
to 20% of patients in psychiatric
hospitals and outpatient clinics.
In clinical settings, about 75% of
persons with the disorder are
women, although this percentage is
lower in community-based samples.
Clinical
Pearls
• How can BPD be
recognized? Recurrent
suicidal threats or acts in
combination with fears of
abandonment are by themselves
strongly indicative of the
diagnosis. The most distinctive
characteristics of patients with
BPD are their hypersensitivity to
rejection and their fearful
preoccupation with expected
abandonment.
•
What is the prognosis for patients
with BPD? While BPD
has long been considered a chronic
and largely untreatable disorder,
more recent data indicate a high
remission rate (about 45% by 2
years and 85% by 10 years), as
defined by meeting fewer than two
criteria for at least 12 months,
and a low relapse rate (about
15%). In other respects, however,
the prognosis remains
discouraging. The suicide rate is
about 8 to 10%, with a
particularly high proportion of
young women. Moreover, even after
remission, most patients with BPD
have severe functional impairment,
with only about 25% of patients
with full-time employment and
about 40% receiving disability
payments after 10 years.
Morning
Report Questions
Q: What is the primary method for
treating BPD? A:
Psychotherapy is the primary
method for treating BPD.
Randomized trials involving
patients with BPD support the
efficacy of several forms of
psychotherapy. The best studied of
these methods is dialectical
behavior therapy.
Q: Is there a role
for pharmacotherapy for patients
with BPD? A: Selective
serotonin-reuptake inhibitors and
other antidepressants are
frequently prescribed to patients
with BPD, but in randomized trials
such drugs have little if any
benefit over placebo. In such
trials, benefits for patients with
BPD have been shown for atypical
antipsychotic agents (e.g.,
olanzapine) and mood stabilizers
(e.g., lamotrigine), particularly
for reducing impulsivity and
aggression. However, these effects
are typically modest, and side
effects are common.
UPDATED
STATISTICS
Borderline Personality Disorder affects
2 out of 50 people, or roughly 4% of the
population, which is 10.8 million people
in the United States.
A whopping 78% of those with BPD
also abuse alcohol, drugs, food, sex,
gambling or some other addictive
practice.
There are approximately 14
million alcoholics in this country, and
3 million of them are recovering in
Alcoholics Anonymous.
Seven (7) million alcoholics have
psychiatric disorders; and of those -
1.8 million people are inflicted with
alcoholism
and Borderline Personality Disorder
(or 26%).
study showed that those with
alcohol use disorders were
3 to 35 times
more likely to be
diagnosed with BPD.
Top
UPDATED
STATISTICS AND FINDINGS
May Is
Borderline Personality Disorder
Awareness Month
from ArticleClover.com
website
Borderline Personality
Disorder (BPD) is an illness often
stemming from a history of childhood
trauma. Disrupted family
relationships, abandonment, sexual
abuse and poor communication within
the family are risk factors for this
devastating disorder. It is
estimated that 5.9% of the general
public struggles with this. People
with BPD have very unstable moods,
swinging from rage to joy and love
to hate in the blink of an eye. They
also have problems with impulse
control. These factors set the stage
for very intense, chaotic
relationships in both the teen years
and into adulthood.
People with Borderline
Personality Disorder view themselves
as victims, accepting little
responsibility for the problems in
their own lives and feel helpless to
change. They commonly see situations
as either good or bad, with no
middle ground. These people also
resist being alone and are extremely
afraid of being disregarded by those
close to them, which may lead them
to mistakenly interpret someone's
behavior as abandonment. Depression,
anxiety and feelings of emptiness
further complicate the situation.
Sadly, people with BPD long for
human connection; however, their
wild mood swings and extremely
impulsive behaviors create tension
in their relationships.
Impulsiveness has been
known to lead to financial problems,
shoplifting, excessive risk taking,
and health problems, including
eating disorders and substance
abuse. Self-mutilation, such as
cutting, scratching or overdosing
are also common in these patients.
Those suffering from
this disorder are often resistant to
treatment, which puts their chances
for normal interaction at risk. BPD
affects more women than men and is
seen more often in psychiatric
patients who have been hospitalized.
Medication to stabilize mood swings
and to lessen the symptoms of
depression is one facet of
treatment. Because authority figures
trigger resistance in people with
BPD, group therapy may be a more
successful route than individualized
therapy. In group therapy, peers are
able to provide support, give
encouragement and are viewed as
equals by the patient.
This disease makes up
20% of all in-patient psychiatric
hospitalizations and 11% of
out-patient psychiatric treatment
programs. One out of 10 people with
BPD will ultimately commit suicide,
which is the most shocking statistic
of all.
Loved ones and family
members trying to support someone
with BPD may be depressed
themselves. Guilt and helplessness
in the face of this illness result
in isolation and a deep sense of
despair. Three-quarters of family
members participating in one online
support group reported themselves as
being in therapy to handle their own
feelings about Borderline
Personality Disorder.
Updated
Statistics
BPD affects
roughly 10 million Americans,
more than 75% of whom are women.
10% of all mental health
outpatients and 20% of inpatients
are thought to have the disorder,
which is characterized by extreme
mood swings, impulsive behavior,
self-injuring acts and suicide
ideation as some of its many
symptoms.
Out
of 1,000 people
-
approximately
40 people are diagnosed
or undiagnosed
Borderlines.
-
Of
those 40, 28 will
attempt suicide one or more
times.
-
Of
those 28, 3 will
be successful
-
0.3%
of the general population will
die a suicide death due to
Borderline Personality
Disorder.
Statistics
for Alcoholics only
from
various sources
-
only
7% of alcoholics who get
sober, stay sober
-
7-10%
commit suicide
-
those
with long-term sobriety, have
5x the probability of
death from
alcoholism.
-
Cause
of Death:
disease 73%, accident
11%, suicide/homicide
7%.
Statistics
for Eating Disorders only
from
many sources
There are 4 categories:
Anorexia, Bulimia, (combinations
of the 2),
Binge Eating Disorder, Food
Addition.
-
82%
of binge eating/food addicts
are effectively treated by
DBT/Cognitive therapy.
-
10%
mortality rate directly from
one of the disorders above.
-
Average
relapse probability is 30%.
Top
|
| |
Brain
scans reveal link
between physical
abuse and psychotic
symptoms in
borderline
personality disorder
from
http://www.healthcanal.com/
A team of scientists
from Cardiff
University and the
University of
Edinburgh have found
that childhood
physical abuse may
increase psychotic
symptoms later in life
for those with the
common psychiatric
condition borderline
personality disorder
(BPD).
Researchers measured the
brain activation of 20
people diagnosed with
BPD and 16 healthy
volunteers in response
to emotional stimuli. In
this case, participants
were shown a series of
photographs of people
with either a neutral or
fearful expression.
The results, published
in Translational
Psychiatry, showed that
there were subtle
behavioural and brain
activation differences
between the two groups
in terms of their
responses to the
emotional faces.
The researchers how the
effects of childhood
experience, specifically
physical abuse and
emotional abuse,
impacted on brain
activation in response
to the fearful faces.
They showed that
individuals with BPD who
had experienced physical
abuse in childhood
activated had greater
activation of the brains
"alerting" system to
emotional stimuli. These
individuals were also
more likely to
experience psychotic
symptoms such as
paranoia and hearing
voices.
"The results of this
study show a significant
association between
childhood trauma and
brain activation in BPD,
and suggest a link
between childhood
physical abuse and
psychotic symptoms in
adulthood" said
Professor Jeremy Hall,
director of the
Neuroscience and Mental
Health Research
Institute at Cardiff
University.
"Overall, it emphasizes
the importance of
continuing biological
research into BPD. This
will help us learn more
about the condition and
to identify suitable
therapies to help those
suffering from it."
Borderline personality
disorder is a common
psychiatric condition,
affecting between 1-3%
of the population. It is
the most prevalent
personality disorder,
and symptoms include
emotional instability
and impulsive behavior.
The research was funded
by the Medical Research
Council (MRC), the
Wellcome Trust and the
Chief Scientist Office
in Scotland. Cardiff
University.
THE CAUSES OF BPD
written
by
a treatment
facility
The
individual suffering
with Borderline
Personality Disorder
typically has a
history of
pathological family
experiences
involving possible
physical, sexual
or/and emotional
abuse, certain
patterns of
over-involvement
between parent and
child, abandonment
by a parent,
inconsistent and
unstable attachment
patterns, poor
emotional support,
neglect, hostility
and lack of
communication within
family environment.
An ‘invalidating
environment’
in childhood has
also been
significantly linked
to Borderline
Personality Disorder
whereupon the
child’s emotional
experiences,
feelings and
expressions are
consistently
dismissed,
belittled,
minimized,
criticized or
ignored. When this
occurs consistently
throughout a child’s
emotional
development, there
can be a thwarting
of the development
of the child’s
emotional self and
ability to know,
understand and
regulate what they
are feeling. This
disruption to their
affective regulation
system and identity
occurs because the
invalidating
environment tells
them that their most
private and innate
experience is wrong
and over time there
is a conflict set up
where the individual
begins to not trust
what they are
feeling and their
self experience
becomes increasingly
distorted.
The expression of
feeling is one of
the most personal
and intrinsic parts
of one’s core self,
who one is, how one
defines themselves
and how they
communicate their
sense of self and
the world to others,
and when a child
does not have their
feelings mirrored
back to them in
order for them to
learn what they are
feeling, but rather
they are
invalidated,
criticized or
rejected, it follows
that there is a base
denial of one’s self
and identity. The
child learns that
their internal
experience is wrong
and inappropriate
and the true self
becomes increasingly
corroded and
disorganized as the
psyche constructs
defenses to deal
with and tolerate
their environment,
often internalizing
the invalidation and
patterns of abuse,
leading them to
often feel like they
are crazy, even if
they are functioning
normally. This leads
these individuals to
often develop
difficulties with
impulse control due
to lacking the
ability to regulate
their emotions and
due to a fragmented
sense of self.
Top
Bullying and
borderline
personality
disorder: a
missing link
from
preventionaction.org website
Bullying
and borderline
personality disorder: a
missing link 04 April
2013 Children abused by
adults are known to be
at increased risk of
developing the serious
and persistent mental
illness known as
borderline
personality-disorder
(BPD). New research
suggests that bullying
and victimization by
other children during
the elementary school
years should be
acknowledged as another
important risk factor.
Psychologists in
Britain, Germany and the
United States base their
conclusions on an
analysis of data from
the Avon Longitudinal
Study of Parents and
Children (ALSPAC) which
has followed the
development of more than
6,000 mothers and
children in south west
England since pregnancy
in the early 1990s.
After
comparing the results of
diagnostic interviews
with the children when
aged 11 with reports of
bullying gathered when
they were aged 8 and 10,
they conclude that
intentional harm
inflicted by peers is a
significant precursor of
BPD symptoms – although
it could be a “marker”
for the increased level
of risk, rather than a
direct cause.
Dieter
Wolke of Warwick
University and his
colleagues note that BPD
is a chronic psychiatric
condition estimated to
affect between 0.7 per
cent and 5.9 per cent of
the adult population.
Its characteristics
include poor mood and
impulse control,
unstable and intense
personal relationships,
and severe difficulty
trusting the actions or
motives of others.
Threats,
rumors and lies
Existing
studies have linked BPD
to childhood experiences
of physical and sexual
abuse, neglect and
exposure to domestic
violence. In addition,
bullying or “peer
victimization” in
childhood has been
associated with the
emergence of psychotic
symptoms and suicidal
thoughts as well as
adverse neurobiological
changes in the brain.
This makes
it all the more
surprising that
potential links with BPD
have not been
investigated before and
that this study is, so
far as the authors know,
the first to use
longitudinal data to
explore the connection.
Wolke and
his colleagues not only
analyzed data collected
from children in the
ALSPAC survey, but also
interviews with parents
and teachers about
victimization when the
children were as young
as 4. Information
gathered on the
children’s home life,
well-being and IQ was
taken into account to
rule out other possible
explanations for the
link between bullying
and BPD symptoms,
including sexual abuse
and harsh, maladaptive
parenting.
The
association between BPD
and different types of
bullying was
investigated by making a
distinction between
“overt victimization”
where victims are
physically hurt or
threatened and
“relational
victimization” involving
exclusion from play by
peers or the circulation
of rumors and lies. The
researchers also
examined “dosage”,
considering whether
bullying was reportedly
chronic or severe.
Pinpointing lessons for
prevention
The
results showed that any
experience of peer
bullying in primary
(elementary) school was
significantly linked to
the emergence of BPD
symptoms in children
under 12. This
association was strong
and remained so even
after controlling the
data for other,
potentially
“confounding”,
explanations.
The study
also found that the risk
of developing symptoms
increased among children
who had experienced
chronic bullying or a
combination of “overt”
and “relational”
victimization. For
children who said they
were victims of both
types of bullying the
odds of BPD symptoms
were increased seven
times compared with
children who were not
bullied. For children
who reported being
bullied at age 8 and
again at age 10, the
odds 5.5 times greater
than for those who had
never been victimized.
Turning
to potential
explanations, the
researchers highlight
the capacity for
bullying to work its way
“under the skin” of its
victims, both
psychologically and
functionally. However,
they also recognize that
children who get bullied
tend to have fewer
friends anyway and are
often more withdrawn,
physically weaker, and
more easily upset than
their peers. Their
victimization could,
consequently, be a
“marker” within a
developmental risk
factor model for BPD,
rather than an actual
cause.
The
development of BPD, as
with other mental health
disorders, is a complex
matter. It is not,
however, difficult to
see why this latest
study – soundly based in
data from a major
longitudinal study –
holds important
implications for
prevention.
At a
universal “whole school”
level, it underlines the
value of applying
structured,
evidence-based
strategies that prevent
victimization and
facilitate swift and
effective action when
bullying occurs. But it
also points to the need
for clinicians working
with children who
already exhibit
significant mental
health problems to be
alert to the links
between BPD and bullying
by peers.
As the
authors of the new study
suggest, professionals
in child and adolescent
mental health should be
routinely asking
children and young
people about
victimization – and be
properly trained to deal
with the answers.
*********
Reference: Wolke, D.,
Schreier, A., Zanarini,
M. C., & Winsper, C.
(2012). Bullied by peers
in childhood and
borderline personality
symptoms at 11 years of
age: A prospective
study. Journal of Child
Psychology and
Psychiatry, 53(8), pp
846-855.
Press Release:
Royal Australian and
NZ College of
Psychiatrists
Psychiatry Congress
highlights
The
Royal Australian and
New Zealand College of
Psychiatrists’
Congress runs until 2
June 2011 at the
Darwin Convention
Centre. The Congress
brings together mental
health experts in a
diverse range of areas
across cultures and
age groups. Here are
some highlights from
today’s program; the
full program is
available at
http://www.ranzcp2011.com/congress-program/.
How
childhood trauma
changes the brain
The brain structure of
children exposed to
chronic trauma and
neglect develops
differently to those
children raised in
secure, healthy,
environments. Drawing
from emerging research
and clinical
experience this
presentation will
examine how exposure
to chronic childhood
stress and terror
results in a brain
hard wired toward a
persistently altered
stress response.
“Children who have
suffered early trauma,
abuse and neglect
commonly have multiple
persistent issues
including poor
emotional regulation,
increased anxiety,
poor problem solving
and impaired social
relationships. If left
untreated these
symptoms can compound
to further social and
health disadvantage in
adulthood,” said
author of this review
Dr Anja Kriegeskotten.
Top
|
|
Invalidation:
What Is Invalidation?
Negates or dismisses
behavior independent
of the actual validity
of the behavior.
To weaken, to nullify,
to cancel, to reject,
to dismiss
What are examples
of invalidating
responses?
1. Reject
self-description
as inaccurate
You
just passed a
difficult math test.
You said that you
feel like Einstein.
Your dad says, “You
don’t know what you
are talking about.”
2. Reject a
normal response.
You
are really into
watching your
favorite show and
don’t feel like
doing your
chores. Your mom
says, “He doesn’t
want to do his
chores because kids
are just brats.”
3. Reject
response to events
as incorrect or
ineffective.
Your
favorite teacher
yelled at you today
and you just told
your sister what
happened. She said,
“That’s stupid to
feel that way. She’s
just a teacher.”
4. Dismiss or
disregard.
Your
beloved dog just was
hit by a car.
Your brother says,
“Oh well, stuff
happens.”
5. Directly
criticize or
punish.
You
are at your
grandpa’s birthday
party. Grandma
cut the cake and you
are passing out the
cake. You
accidentally drop a
one of the plates.
Grandma says, “You
idiot. You don’t
need birthday cake
if you just smear it
all over my floor.”
6. Reject and
link responses to
socially
unacceptable
characteristics.
You
are helping your
grandpa in the
garage. One of
the bigger tools
just fell on your
fingers. Your
grandpa says,
“Crying means you
are weak. Suck it
up.”
How does
invalidation
impact us?
1.
Confusion about
self: learns not to
trust self and
relies on social
environment for the
correct response.
2. Problems
regulating emotions:
Ignores or withholds
emotions or is
extremely emotional.
3.
Oversimplification:
Highly sensitive to
failure,
perfectionism, and
forms unrealistic
goals.
4. Responses to and
view of the world
are not accurate.
5. Look to others to
tell you how to do
things.
Back to
Environment
|
|
|
The
following is from Dr.
Shapiro's website under the
link, "What is EMDR?" Dr.
Francine Shapiro is founder
of EMDR Therapy.
"Eye Movement Desensitization
and Reprocessing"
(EMDR) is a comprehensive,
integrative psychotherapy
approach. It contains elements
of many effective
psychotherapies in structured
protocols that are designed to
maximize treatment effects.
These include psychodynamic,
cognitive behavioral,
interpersonal, experiential, and
body-centered therapies2.
EMDR is an information
processing therapy and uses an
eight phase approach to address
the experiential contributors of
a wide range of pathologies. It
attends to the past experiences
that have set the groundwork for
pathology, the current
situations that trigger
dysfunctional emotions, beliefs
and sensations, and the positive
experience needed to enhance
future adaptive behaviors and
mental health.
During treatment various
procedures and protocols are
used to address the entire
clinical picture. One of the
procedural elements is "dual
stimulation" using either
bilateral eye movements, tones
or taps. During the reprocessing
phases the client attends
momentarily to past memories,
present triggers, or anticipated
future experiences while
simultaneously focusing on a set
of external stimulus. During
that time, clients generally
experience the emergence of
insight, changes in memories, or
new associations. The clinician
assists the client to focus on
appropriate material before
initiation of each subsequent
set.
Eight Phases of Treatment
The 1st phase is a history
taking session during which the
therapist assesses the client's
readiness for EMDR and develops
a treatment plan. Client and
therapist identify possible
targets for EMDR processing.
These include recent distressing
events, current situations that
elicit emotional disturbance,
related historical incidents,
and the development of specific
skills and behaviors that will
be needed by the client in
future situations.
During 2nd phase of treatment,
the therapist ensures that the
client has adequate methods of
handling emotional distress and
good coping skills, and that the
client is in a relatively stable
state. If further stabilization
is required, or if additional
skills are needed, therapy
focuses on providing these. The
client is then able to use
stress reducing techniques
whenever necessary, during or
between sessions. However, one
goal is not to need these
techniques once therapy is
complete.
In phases 3-6, a target is
identified and processed using
EMDR procedures. These involve
the client identifying the most
vivid visual image related to
the memory (if available), a
negative belief about self,
related emotions and body
sensations. The client also
identifies a preferred positive
belief. The validity of the
positive belief is rated, as is
the intensity of the negative
emotions.
After this, the client is
instructed to focus on the
image, negative thought, and
body sensations while
simultaneously moving his/her
eyes back and forth following
the therapist's fingers as they
move across his/her field of
vision for 20-30 seconds or
more, depending upon the need of
the client. Although eye
movements are the most commonly
used external stimulus,
therapists often use auditory
tones, tapping, or other types
of tactile stimulation. The kind
of dual attention and the length
of each set is customized to the
need of the client. The client
is instructed to just notice
whatever happens. After this,
the clinician instructs the
client to let his/her mind go
blank and to notice whatever
thought, feeling, image, memory,
or sensation comes to mind.
Depending upon the client's
report the clinician will
facilitate the next focus of
attention. In most cases a
client-directed association
process is encouraged. This is
repeated numerous times
throughout the session. If the
client becomes distressed or has
difficulty with the process, the
therapist follows established
procedures to help the client
resume processing. When the
client reports no distress
related to the targeted memory,
the clinician asks him/her to
think of the preferred positive
belief that was identified at
the beginning of the session, or
a better one if it has emerged,
and to focus on the incident,
while simultaneously engaging in
the eye movements. After several
sets, clients generally report
increased confidence in this
positive belief. The therapist
checks with the client regarding
body sensations. If there are
negative sensations, these are
processed as above. If there are
positive sensations, they are
further enhanced.
In phase 7, closure, the
therapist asks the client to
keep a journal during the week
to document any related material
that may arise and reminds the
client of the self-calming
activities that were mastered in
phase two.
The next session begins with
phase 8, re-evaluation of the
previous work, and of progress
since the previous session. EMDR
treatment ensures processing of
all related historical events,
current incidents that elicit
distress, and future scenarios
that will require different
responses. The overall goal is
produce the most comprehensive
and profound treatment effects
in the shortest period of time,
while simultaneously maintaining
a stable client within a
balanced system.
After EMDR processing, clients
generally report that the
emotional distress related to
the memory has been eliminated,
or greatly decreased, and that
they have gained important
cognitive insights. Importantly,
these emotional and cognitive
changes usually result in
spontaneous behavioral and
personal change, which are
further enhanced with standard
EMDR procedures.
Top
Back to EMDR
Mount
Sinai researchers have found that
real-time brain imaging suggests
that patients with Borderline
Personality Disorder (BPD) are
physically unable to activate
neurological networks that can
help regulate emotion. The
findings, by Harold W.
Koenigsberg, MD, Professor of
Psychiatry at Mount Sinai School
of Medicine, were presented at the
11th International Congress of the
International Society for the
Study of Personality Disorders
(ISSPD), held August 21-23, 2009
at The Mount Sinai Medical Center
in New York. The research will
also be published in the journal Biological
Psychiatry.
Using functional magnetic
resonance imaging (MRI), Dr.
Koenigsberg observed how the
brains of people with BPD reacted
to social and emotional stimuli.
He found that when people with BPD
attempted to control and reduce
their reactions to disturbing
emotional scenes, the anterior
cingulated cortex and
intraparetical sulci areas of the
brain that are active in healthy
people under the same conditions
remained inactive in the BPD
patients.
"This research shows that BPD
patients are not able to use those
parts of the brain that healthy
people use to help regulate their
emotions," said Dr. Koenigsberg.
"This may explain why their
emotional reactions are so
extreme.
Gene function and serotonin
levels may also be contributing
factors in BPD, according to
research findings also presented
at the ISSPD Congress by Larry
Siever, MD, Professor of
Psychiatry and Director of the
Special Evaluation Program for
Mood and Personality Disorders
at Mount Sinai School of
Medicine. Dr. Siever's research
demonstrates how genes related
to serotonin and neuropeptides
in the brain may be altered in
serious personality disorders
such as BPD.
Dr. Siever's neuro-imaging
research suggests that a gene
that controls production of a
critical enzyme for the
synthesis of serotonin, a brain
chemical that modulates emotions
and aggression, may be altered
leading to reduced synthesis of
serotonin in people with BPD and
may be associated with increased
aggression. This variant of gene
may also be associated with
reduced frontal lobe activation
in the brain.
These studies were part of the
11th International Congress of
the International Society for
the Study of Personality
Disorders, which took place
August 21 - 23, 2009 at The
Mount Sinai Medical Center in
New York.
Return to General
Info
Top
REDUCING THE SEVERITY OF
BPD
By
SHARI ROAN, LOS
ANGELES TIMES
The primary
treatments for borderline
personality disorder are
behavioral strategies, such as
dialectical behavioral therapy,
which University of Washington
psychologist Marsha Linehan
devised almost two decades ago.
In
this approach, the patients
acknowledge that they have damaged
their relationships while learning
to regulate their emotions and
change their most destructive
behaviors. It takes time and
effort.
"It's
very active. It's not talk
therapy," Linehan says. Instead of
just talking about the fact that
she is always arguing with people,
for example, the patient has to
try to find something to agree on
with someone she is arguing with.
There
are other successful therapies,
such as mentalization-based
therapy, which focuses on
observing one's own emotions and
those of other people in order to
understand the effect of emotions,
and transference-focused therapy,
which centers on helping the
patient develop new skills that
overcome the tendency to see
everything in extremes.
And
studies show that these
very specific behavioral
therapies can reduce
some of the most severe
behaviors.
A 2006
study in the Archives of
General Psychiatry
showed that suicidal
patients who were
randomized to
dialectical behavior
therapy were half as
likely to make future
suicide attempts
compared to patients who
were treated with more
conventional therapies.
A study
published in May in the
American Journal of
Psychiatry showed that
patients treated with
mentalization-based
therapy (MBT) had
sustained improvements
in their symptoms
compared to patients
undergoing conventional
treatment.
And
research in the same
journal, published in
2007, found that
patients undergoing
transference-focused
therapies, dialectical
behavior therapy and
other supportive
therapies showed
improvements in
depression, anxiety,
daily functioning and
social adjustment after
one year of
treatment.
Top
Conclusion
|
|
How
a Borderline Personality
Disorder Love Relationship
Evolves
Article:
Adapted from Romeo's Bleeding by
Roger Melton, M.A.
Regardless of how a person with
Borderline Personality Disorder
alters and tailor her appearance
and actions to please others, she
often presents with a clear and
characteristic personality pattern
over time. This pattern usually
evolves through three stages: The
Vulnerable Seducer, The Clinger,
and The Hater. This evolution may
take months, and sometimes even
years to cycle through. In the
later periods, the personality
often swings wildly back and forth
from one phase to the next.
Love: The
Vulnerable Seducer Phase
At first, a
Borderline female may appear
sweet, shy, vulnerable and
"ambivalently in need of being
rescued"; looking for her Knight
in Shining Armor.
In the beginning,
you will feel a rapidly
accelerating sense of compassion
because she is a master at
portraying herself as she "victim
of love" and you are saving her.
But listen closely to how she sees
herself as a victim. As her
peculiar emotional invasion
advances upon you, you will hear
how no one understands her -
except you. Other people have been
"insensitive." She has been
betrayed, just when she starts
trusting people. But there is
something "special" about you,
because "you really seem to know
her."
It is this intense
way she has of bearing down on you
emotionally that can feel very
seductive. You will feel elevated,
adored, idealized - almost
worshiped, maybe even to the level
of being uncomfortable. And you
will feel that way quickly. It may
seem like a great deal has
happened between the two of you in
a short period of time, because
conversation is intense, her
attention, and her eyes are so
deeply focused on you.
Here is a woman who
may look like a dream come true.
She not only seems to make you the
center of her attention, but she
even craves listening to your
opinions, thoughts and ideas. It
will seem like you have really
found your heart's desire.
Like many things
that seems too good to be true,
this is. This is borderline
personality disorder.
It will all seem so
real because it is real in her
mind. But what is in her mind it
is not what you perceive to be
happening.
Love: The Clinger
Phase
Once she has
successfully candied her hook with
your adoration, she will weld it
into place by “reeling in” your
attention and concern. Her intense
interest in you will subtly
transform over time. She still
appears to be interested in you,
but no longer in what you are
interested in. Her interest
becomes your exclusive interest in
her. This is when you start to
notice “something”. Your thoughts,
feelings and ideas fascinate her,
but more so when they focus on
her. You can tell when this
happens because you can feel her
"perk-up" emotionally whenever
your attention focuses upon her
feelings and issues. Those moments
can emotionally hook your
compassion more deeply into her,
because that is when she will
treat you well - tenderly.
It’s often here, you
begin to confuse your empathy with
love, and you believe you're in
love with her. Especially if your
instinct is strong and rescuing is
at the heart of your "code."
Following that code results in the
most common excuse I hear as a
therapist, as to why many men stay
with borderline women, ".... But I
love her!" Adult love is built on
mutual interest, care and respect
- not on one-way emotional
rescues. And mothering is for
kids. Not grown men.
But, if like King
Priam, you do fall prey to this
Trojan Horse and let her inside
your city gates, the first
Berserker to leave the horse will
be the devious Clinger. A master
at strengthening her control
through empathy, she is brilliant
at eliciting sympathy and
identifying those most likely to
provide it-like the
steady-tempered and tenderhearted.
The world ails her.
Physical complaints are common.
Her back hurts. Her head aches.
Peculiar pains of all sorts come
and go like invisible, malignant
companions. If you track their
appearance, though, you may see a
pattern of occurrence connected to
the waning or waxing of your
attentions. Her complaints are
ways of saying, "don't leave me.
Save me!" And Her maladies are not
simply physical. Her feelings ail
her too.
She is depressed or
anxious, detached and indifferent
or vulnerable and hypersensitive.
She can swing from elated
agitation to mournful gloom at the
blink of an eye. Watching the
erratic changes in her moods is
like tracking the needle on a
Richter-scale chart at the site of
an active volcano, and you never
know which flick of the needle
will predict the big explosion.
But after every
emotional Vesuvius she pleads for
your mercy. And if she has
imbedded her guilt-hooks deep
enough into your conscientious
nature, you will stay around and
continue tracking this volcanic
earthquake, caught in the illusion
that you can discover how to stop
Vesuvius before she blows again.
But, in reality, staying around
this cauldron of emotional
unpredictability is pointless.
Every effort to understand or help
this type of woman is an
excruciatingly pointless exercise
in emotional rescue.
It is like you are a
Coast Guard cutter and she is a
drowning woman. But she drowns in
a peculiar way. Every time you
pull her out of the turbulent sea,
feed her warm tea and biscuits,
wrap her in a comfy blanket and
tell her everything is okay, she
suddenly jumps overboard and
starts pleading for help again.
And, no matter how many times you
rush to the emotional - rescue,
she still keeps jumping back into
trouble. It is this repeating,
endlessly frustrating pattern
which should confirm to you that
you are involved with a Borderline
Personality Disorder. No matter
how effective you are at helping
her, nothing is ever enough. No
physical, financial or emotional
assistance ever seems to make any
lasting difference. It's like
pouring the best of your self into
a galactic-sized Psychological
Black Hole of bottomless emotional
hunger. And if you keep pouring it
in long enough, one-day you'll
fall right down that hole
yourself. There will be nothing
left of you but your own shadow,
just as it falls through her
predatory "event horizon." But
before that happens, other signs
will reveal her true colors.
Sex will be
incredible. She will be
instinctually tuned in to reading
your needs. It will seem wonderful
- for a while.
The intensity of her
erotic passion can sweep you away,
but her motive is double-edged.
One side of it comes from the
instinctually built-in, turbulent
emotionality of her disorder.
Intensity is her trump-card.
But the other side
of her is driven by an equally
instinctually and concentrated
need to control you. The sexual
experiences, while imposing, are
motivated from a desire to
dominate you, not please you. Her
erotic intensity will be there in
a cunning way tailored so you will
not readily perceive it.
“I love you” means –
“I need you to love me”. “That was
the best ever for me” means – tell
me “it was the best ever for you”.
Show me that I have you.
Love: The Hater
Phase
Once a Borderline
Controller has succeeded and is in
control, the Hater appears. This
hateful part of her may have
emerged before, but you probably
will not see it in full, acidic
bloom until she feels she has
achieved a firm hold on your
conscience and compassion. But
when that part makes it's first
appearance, rage is how it breaks
into your life.
What gives this rage
its characteristically borderline
flavor is that it is very
difficult for someone witnessing
it to know what triggered it in
reality. But that is its primary
identifying clue: the actual
rage-trigger is difficult for you
to see. But in the Borderline's
mind it always seems to be very
clear. To her, there is always a
cause. And the cause is always
you. Whether it is the tone of
your voice, how you think, how you
feel, dress, move or breathe - or
"the way you're looking at me," -
she will always justify her rage
by blaming you for "having to hurt
her."
Rage reactions are
also unpredictable and unexpected.
They happen when you least expect
it. And they can become extremely
dangerous. It all serves to break
you down over time. Your self
esteem melts away. You change and
alter your behavior in hopes of
returning to the “Clinger Stage”.
And periodically you will, but
only to cycle back to the hater
when you least expect it, possibly
on her birthday, or your
anniversary.
Borderline
Personality Disorder is a serious
mental illness.
Back
to Relationship Recovery
Top
|
|
Love When You
have Borderline Personality
Disorder...
Some partners of people with BPD
worry the relationship was just a
game, that their SO was using them
and felt nothing for them. That’s
not true.
I
am a recovering BP.
Before,
when I was in a relationship, my
feelings felt genuine. I didn’t
have a conscious ulterior motive.
There was an authentic connection;
and while it may have been
unhealthy and for the wrong
reasons, it was, in my mind, real.
I
acted as if I was in love because
I thought I was.
The
bond that occurred in the
beginning of a relationship was
incredible: there was a deep
(false) sense of knowing the other
person intimately, intuitively. He
became my whole world and it was
wonderful, rapturous. When my
boyfriends left – and they
invariably left – that world was
annihilated; everything fell to
ashes.
The
breakup that led to my hard-won
recovery from BPD left me
literally slumped on the floor,
crushed in spirit, feeling as if
there was no meaning in my life.
I
was close to killing myself - too
defeated and broken to even move.
The saddest thing about the
situation was that I was the cause
of my pain, yet had little idea
then that it was due to my own
behavior.
So
yes, the love is “real”, but only
in the sense of how it feels to
the person with BPD: the feelings
seem real, they feel like love.
But it’s not love
because it’s based on need rather
than on true caring and intimacy,
which is the real love we all
deserve. ~Oceanheart
Back
to Relationship Recovery
Top
|
|
The Five
Stages of Discovery for Family
Members elsewhere
in site
Paul
Mason. MS, CPC, and Randi Kreger,
Excerpt from "Stop Walking on
Eggshells"
A Family Members Discovery and
Reaction to Borderline Personality
Disorder
People who love someone with
Borderline Personality Disorder seem
to go through similar stages in their
discovery and learning about the
disorder and the recovery of their own
lives. The longer the relationship has
lasted, the longer each stage seems to
take. Although these stages are listed
in the general order in which people
go experience them, most people move
back and forth among the different
stages.
Confusion Stage
This generally occurs before a
diagnosis of Borderline Personality
Disorder is known. Family members
struggle to understand why Borderlines
sometimes behave in ways that seem to
make no sense. They look for solutions
that seem elusive, blame themselves,
or resign themselves to living in
chaos. Even after learning about BPD,
it can take family members (sometimes
referred to as "non-BPD's) weeks or
months to really comprehend on an
intellectual level how the Borderline
Person is personally affected by this
complex disorder. It can take even
longer to absorb the information on an
emotional level.
Outer-Directed Stage -
Focuses on the Person with BPD
In this stage, non-BPD's turn their
attention toward the person with the
disorder, urging them to seek
professional help, attempting to get
them to change, and trying their best
not to trigger problematic behavior.
People at this stage usually learn all
they can about BPD in an effort to
understand and empathize with the
person they care about. It can take
family members a long time to
acknowledge feelings of anger and
grief--especially when the Borderline
Person is a parent or child. Anger is
an extremely common reaction, even
though most family members understand
on an intellectual level that
Borderline Personality Disorder is not
the borderline's fault. Yet because
anger seems to be an inappropriate
response to a situation that may be
beyond the borderline's control,
family members often suppress their
anger and instead experience
depression, hopelessness, and guilt.
The chief tasks for family members in
this stage include acknowledging and
dealing with their own emotions,
letting the Borderline Person take
responsibility for their own actions,
and giving up the fantasy that the
Borderline Person will behave as the
family members would like them to.
Inner-Directed Stage
- Focus on Ones Self
Eventually, family members look inward
and conduct an honest appraisal of
themselves. It takes two people to
have a relationship, and the goal for
family members in this stage is to
better understand their role in making
the relationship what it now is. The
objective here is not
self-recrimination, but insight and
self-discovery.
Decision-Making
Stage
Armed with knowledge and insight,
family members struggle to make
decisions about the relationship. This
stage can often take months or years.
Family members in this stage need to
clearly understand their own values,
beliefs, expectations, and
assumptions. For example, one man with
a physically violent borderline wife
came from a conservative family that
strongly disapprove of divorce. His
friends counseled him to separate from
her, but he felt unable to do so
because of his concern about how his
family would react. You may find that
your beliefs and values have served
you well throughout your life. Or you
may find that you inherited them from
your family without determining
whether or not they truly reflect who
you are. Either way, it is important
to be guided by your own values--not
someone else's.
Resolution Phase
In this final stage, family members
implement their decisions and live
with them. Depending upon the type of
relationship, some family members may,
over time, change their minds many
times and try different alternatives.
When it comes to chosen
relationships, we found that the
Borderline Person's willingness to
admit they had a problem and seek help
was by far the determining factor as
to whether the couple stayed together
or not... If you are looking at this
right now, know that you are not
alone.
Back
to Relationship Recovery
Top
Brain
Abnormalities Underlying Key
Element Of Borderline
Personality Disorder
Identified
ScienceDaily
—
Using new approaches, an
interdisciplinary team of
scientists at
NewYork-Presbyterian
Hospital/Weill Cornell Medical
Center in New York City has
gained a view of activity in
key brain areas associated
with a core difficulty in
patients with borderline
personality disorder—shedding
new light on this serious
psychiatric condition.
"In its
early days yet, but
the work is
pinpointing functional
differences in the
neurobiology of
healthy people versus
individuals with the
disorder as they
attempt to control
their behavior in a
negative emotional
context. Such initial
insights can help
provide a foundation
for better, more
targeted therapies
down the line,"
explains lead
researcher Dr. David
A. Silbersweig, the
Stephen P. Tobin and
Dr. Arnold M. Cooper
Professor of
Psychiatry and
Professor of Neurology
at Weill Cornell
Medical College, and
attending psychiatrist
and neurologist at
NewYork-Presbyterian
Hospital/Weill Cornell
Medical Center.
Borderline
personality disorder
is a devastating
mental illness that
affects between 1 to 2
percent of Americans,
causing untold
disruption of
patients' lives and
relationships.
Nevertheless, its
underlying biology is
not very well
understood. Hallmarks
of the illness include
impulsivity, emotional
instability,
interpersonal
difficulties, and a
preponderance of
negative emotions such
as anger—all of which
may encourage or be
associated with
substance abuse,
self-destructive
behaviors and even
suicide.
"In this
study, our
collaborative team
looked specifically at
the nexus between
negative emotions and
impulsivity—the
tendency of people
with borderline
personality disorder
to 'act out'
destructively in the
presence of anger,"
Dr. Silbersweig
explains. "Other
studies have looked at
either negative
emotional states or
this type of
behavioral
disinhibition. The two
are closely connected,
and we wanted to find
out why. We therefore
focused our
experiments on the
interaction between
negative emotional
states and behavioral
inhibition."
Advanced
brain-scanning
technologies developed
by the research team
made it possible to
detect the brain areas
of interest with
greater sensitivity.
"Previous
work by our group and
others had suggested
that an area at the
base of the brain
within the
ventromedial
prefrontal cortex was
key to people's
ability to restrain
behaviors in the
presence of emotion,"
Dr. Silbersweig
explains.
Unfortunately,
tracking activity in
this brain region has
been extremely
difficult using
functional MRI (fMRI).
"Due to its particular
location, you get a
lot of signal loss,"
the researcher
explains.
However,
the Weill Cornell team
used a special fMRI
activation probe that
they developed to
eliminate much of that
interference. This
paved the way for the
study, which included
16 patients with
borderline personality
disorder and 14
healthy controls.
The team
also used a tailored
fMRI
neuropsychological
approach to observe
activity in the
subjects' ventromedial
prefrontal cortex as
they performed what
behavioral
neuroscience
researchers call
"go/no go" tests.
These
rapid-fire tests
require participants
to press or withhold
from pressing a button
whenever they receive
particular visual
cues. In a twist from
the usual approach,
the performance of the
task with negative
words (related to
borderline psychology)
was contrasted with
the performance of the
task when using
neutral words, to
reveal how negative
emotions affect the
participants' ability
to perform the task.
As
expected, negative
emotional words caused
participants with
borderline personality
disorder to have more
difficulty with the
task at hand and act
more
impulsively—ignoring
visual cues to stop as
they repeatedly
pressed the button.
But what
was really interesting
was what showed up on
MRI.
"We
confirmed that
discrete parts of the
ventromedial
prefrontal cortex—the
subgenual anterior
cingulate cortex and
the medial
orbitofrontal cortex
areas—were relatively
less active in
patients versus
controls," Dr.
Silbersweig says.
"These areas are
thought to be key to
facilitating
behavioral inhibition
under emotional
circumstances, so if
they are
underperforming that
could contribute to
the disinhibition one
so often sees with
borderline personality
disorder."
At the
same time, the
research team observed
heightened levels of
activation during the
tests in other areas
of the patients'
brains, including the
amygdala, a locus for
emotions such as anger
and fear, and some of
the brain's other
limbic regions, which
are linked to
emotional processing.
"In the
frontal region and the
amygdala, the degree
to which the brain
aberrations occurred
was closely correlated
to the degree with
which patients with
borderline personality
disorder had clinical
difficulty controlling
their behavior, or had
difficulty with
negative emotion,
respectively," Dr.
Silbersweig notes.
The
study sheds light not
only on borderline
personality disorder,
but on the mechanisms
healthy individuals
rely on to curb their
tempers in the face of
strong emotion.
Still,
patients struggling
with borderline
personality disorder
stand to benefit most
from this
groundbreaking
research. An
accompanying journal
commentary labels the
study "rigorous" and
"systematic," and one
of the first to
validate with
neuroimaging what
scientists had only
been able to guess at
before.
"The
more that this type
of work gets done,
the more people will
understand that
mental illness is
not the patient's
fault—that there are
circuits in the
brain that control
these functions in
humans and that
these disorders are
tied to fundamental
disruptions in these
circuits," Dr.
Silbersweig says.
"Our hope is that
such insights will
help erode the
stigma surrounding
psychiatric
illness."
Back
to General
Info.
Borderline
Personality
Disorder
Caused by
Genetic
Material on
Chromosome
9
by Dr.
Giuseppe
Spezzano C.
Psych. in
Mental Health
Recent
research from
the National
Institute of
Mental Health
indicates that
“genetic
material on
chromosome
nine was
linked to BPD
features”.
This research,
while
valuable, is
misleading
(more on that
later). First,
what is
Borderline
Personality
Disorder?
People who
experience BPD
are highly
emotionally
reactive and
their moods,
interpersonal
relationships,
self-image and
behavior are
very unstable
and erratic.
Their black
and white
thinking
patterns are
reflected in
their tendency
to idealize
others and
then become
extremely
disillusioned
with that same
person due to
acute
abandonment
fears.
Self-harm,
suicidal
thoughts,
eating
disorders, and
alcohol and
drug abuse are
some of the
typical
co-occurring
difficulties.
According to
this new
research,
“genetic
factors play a
major role in
individual
differences of
borderline
personality
disorder
features in
Western
society”. What
is not
mentioned in
the article is
the fact that
40 to 71
percent of
people
diagnosed with
BPD have been
abused as
children. The
article also
fails to
mention that
75% of people
diagnosed with
BPD are
female. While
a number of
factors may
contribute to
the
development of
BPD, the role
of childhood
physical,
sexual and
emotional
abuse, and the
fact that it
is seen
predominantly
in women, is
neither new or
controversial
and should be
mentioned as
part of the
BPD context.
Not mentioning
these long
established
facts creates
a false
impression,
and a
misguided hope
for a genetic
cure. It also
neglects the
painful
background
experiences
plaguing
people who
experience BPD
and takes the
focus off
abuse
prevention
and the need
to support
abuse victims
who wish to
come forward.
Back
to
Genetics
I recently was
blessed with
the
opportunity to
talk with
author,
psychologist,
and science
journalist
Daniel Goleman
about his new
book,
The Brain
and Emotional
Intelligence:
New Insights.
Among
Goleman's
prolific body
of work is the
best-selling
book
Emotional
Intelligence:
Why It Can
Matter More
Than IQ,
a subject that
he has
revisited and
expanded upon
in his newest
offering.
Tricycle:
How does
understanding
the brain help
us manage
stress?
Daniel Goleman:
There are
several ways
that
understanding
some brain
mechanics and
having basic
neural tools
at hand can
help us manage
stress. First
of all, we
have to
realize that
there’s no
escaping
stress
completely;
this is the
nature of
life. Some of
what's called
samsara is
what other
people call
“stress”. When
we're stressed
the part of
the brain that
takes over,
the part that
reacts the
most, is the
circuitry that
was originally
designed to
manage
threats—especially
circuits that
center on the
amygdala,
which is in
the emotional
centers of the
brain.
The amygdala
is the trigger
point for the
fight, flight,
or freeze
response. When
these circuits
perceive a
threat, they
flood the body
with stress
hormones that
do several
things to
prepare us for
an emergency.
Blood shunts
away from the
organs to the
limbs; that’s
the fight or
flee. But the
response is
also
cognitive—and,
in modern life
this is what
matters most,
it makes some
shifts in how
the mind
functions.
Attention
tends to
fixate on the
thing that is
bothering us,
that’s
stressing us,
that we're
worried about,
that’s
upsetting,
frustrating,
or angering
us. That means
that we don’t
have as much
attentional
capacity left
for whatever
it is we're
supposed to be
doing or want
to be doing.
In addition,
our memory
reshuffles its
hierarchy so
that what's
most relevant
to the
perceived
threat is what
comes to mind
most
easily—and
what's deemed
irrelevant is
harder to
bring to mind.
That, again,
makes it more
difficult to
get things
done than we
might want.
Plus, we tend
to fall back
on
over-learned
responses,
which are
responses
learned early
in life—which
can lead us to
do or say
things that we
regret later.
It is
important to
understand
that the
impulses that
come to us
when we're
under
stress—particularly
if we get
hijacked by
it—are likely
to lead us
astray.
It's extremely
important to
widen the gap
between
impulse and
action; and
that’s exactly
what
mindfulness
does. This is
one of the big
advantages of
mindfulness
practice: it
gives us a
moment or two,
hopefully,
where we can
change our
relationship
to our
experience,
not be caught
in it and
swept away by
impulse, but
rather to see
that there's
an opportunity
here to make a
different,
better choice.
I think that
understanding
the basic
neural
mechanisms
involved is an
aid to
mindfulness
because it
tells us we
don’t have to
get swept
away.
Tricycle:
Fascinating.
It seems that
it is through
awareness that
we have any
choice at all,
as opposed to
just letting
our reactions
dictate
everything we
do.
Daniel Goleman:
Yes, exactly,
the
unconscious
mind is
completely
happy to make
all of our
decisions for
us, and to run
us on
“automatic,”
through
habitual
sequences that
roll on
outside of our
awareness—and
so without our
seeing that a
choice was
even there to
be made. When
we are
mindless, so
to speak,
we're piloted
through our
day seemingly
by whim, by
pure habit.
Mindfulness
lets us step
out of that
rut and see
that there's
another road
we could take
and actually
take that
road. So it's
a very
powerful
choice point
in the mind.
Tricycle:
We have quite
a capacity for
autopilot, it
seems.
Daniel Goleman:
Yes, exactly.
Tricycle:
So stress
reactions and
various
difficulties
are hardwired
into the
brain, so to
speak. I'm
curious—are
ethics or
morality
hardwired into
our brains as
well?
Daniel Goleman:
There's some
evolutionary
thinking that
there tend to
be four or
five universal
dimensions of
ethics and
ethical
choice, but no
one is saying
there’s some
specific spot
in the brain
which is our
ethical
center. It’s
certainly more
diffuse than
that.
The
psychologist
Jonathan Haidt
proposes an
evolutionary
theory that
there are five
or so
universal
dimensions of
ethics. He has
written about
how universal,
for example, a
sense of
fairness seems
to be, or the
positive value
of cleanliness
and negativity
of dirtiness,
or a concern
with larger
meanings. So,
it may be that
our brain is
designed to
foster our
thinking about
such ethical
concerns. I
don’t know if
you could say
it's hardwired
but I think
the capacity
for ethical
concerns seems
to be a
universal
brain
function.
Tricycle:
How do you
feel about all
the time that
we're spending
online these
days? How
might this
effect our
brains?
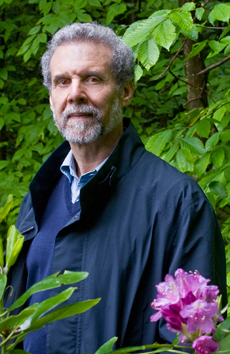 Daniel
Goleman:
I think it's
an enormous
experiment
with our sense
of community
and our
children.
Evolution
designed the
human brain
for
face-to-face
human contact,
particularly
our capacity
for empathy,
which, of
course, is
very strongly
related to our
sense of
ethics.
Empathy is the
essential
factor for
compassion but
online we may
be disabling
this. The
social centers
of the brain
seem to act
like an
interpersonal
radar attuning
to the person
we're with,
and activating
in our own
brain what's
going on with
that
person—their
feelings,
their
intentions,
their
movements.
Because we
have this
inner sense of
what they're
doing we don’t
have to think
about it; this
is another
automatic
function. Daniel
Goleman:
I think it's
an enormous
experiment
with our sense
of community
and our
children.
Evolution
designed the
human brain
for
face-to-face
human contact,
particularly
our capacity
for empathy,
which, of
course, is
very strongly
related to our
sense of
ethics.
Empathy is the
essential
factor for
compassion but
online we may
be disabling
this. The
social centers
of the brain
seem to act
like an
interpersonal
radar attuning
to the person
we're with,
and activating
in our own
brain what's
going on with
that
person—their
feelings,
their
intentions,
their
movements.
Because we
have this
inner sense of
what they're
doing we don’t
have to think
about it; this
is another
automatic
function.
Tricycle:
Like mirror
neurons?
Daniel Goleman:
Mirror neurons
are one of the
main classes
of neurons
that have been
discovered in
the social
brain—all of
these social
circuits
together keep
things
operating
smoothly
during
interactions.
But when we're
online there's
no channel for
our social
brain to get
feedback. The
mirror neurons
have nothing
to read, and
so we're
operating in
the dark. This
may create,
for example, a
negativity
bias to email,
where the
sender thinks
the message is
more positive
than does the
person who
receives. This
also means
people are
more likely to
experience
what's called
“cyber-disinhibition”
which means
that, say,
you're having
a little bit
of an
emotional
hijack and if
you were
face-to-face
your social
circuitry
might tell you
"Well, it
would be
better to say
this than
that." In
other words,
you might be
artful about
it. But online
it has zero
feedback;
that’s the
disinhibition
which gives
rise to what's
called
flaming.
Flaming is
when
somebody's
really
agitated and
they sit down
and pound out
a message all
in caps, and
they hit
"send" and
then
immediately
regret it;
it's a classic
online hijack.
So, on the
downside,
there also may
be some
emotional
numbing, some
deadening of
empathy, and
all of that
means that we
may be fraying
social
connections as
more and more
interactions
become virtual
as on Facebook
and less and
less
face-to-face.
Then there is
the big
experiment
that is
perhaps the
most
troubling:
kids are
spending more
and more time
during
childhood
online. This
changes the
way we have
always taught
social and
emotional
skills in
life, in
day-to-day
interactions.
If kids are
spending fewer
hours of time
together in
person and
more and more
hours online
we might be
de-skilling
entire
generations in
essentials for
a full human
life.
Tricycle:
Do you
recommend any
practices or
activities
that might
help people
living in this
age develop
their capacity
for emotional
intelligence?
Daniel Goleman:
The good news
is that there
are ways to
cultivate
emotional
intelligence.
But first
remember that
emotional
intelligence
is a set of
human skills;
it is not one
monolithic
ability. It
includes
self-awareness,
it includes
managing your
emotions (or
“self-regulation)
which doesn’t
mean
suppressing
emotions, but
not letting
your
disturbing
emotions get
in the way of
life and also
marshalling
your positive
emotions and
passions for a
full life.
Third is
empathy,
sensing how
other people
are feeling
and a general
social
awareness, and
fourth,
putting that
all together
in social
skill during
interactions.
I would say
that there are
many aspects
of dharma
practice that
would
facilitate
different
parts of
emotional
intelligence.
Tonglen
practice, for
example, is
explicitly
attuning into
the other
person and I
think that
must
strengthen
empathy. I
have yet to
see the
research study
that shows
that but I
would bet that
that’s what it
would find. I
also think
that the
ethical
dimension of
dharma
practice is
implemented by
strengthening
our
self-regulation,
and I think
that
meditation
practice
generally is a
way to enhance
self-awareness.
So I can see
many, many
ways in which
dharma
practice
itself could
give a boost
to different
aspects of
emotional
intelligence.
Tricycle:
Can you talk
about the
relationship
between
motivation and
emotion?
Daniel Goleman:
Motivations
are drivers of
positive
emotion. When
we do the
things we are
motivated to
do, and some
people are
motivated to
have strong
connections
with other
people, those
things will
give us a kind
of spontaneous
high. Some
people are
motivated to
strive
incessantly
for
achievement,
while some
people are
motivated to
exert power by
influencing
other people,
some for the
better, some
for the worse.
So, I think
that the
relationship
is that one is
the driver of
the other. Our
motives
determine what
we enjoy. Our
values, on the
other hand,
are a little
different from
our
motivations.
Our values are
our sense of
what we should
do and what we
should like
and it's
clearly best
to be in a
situation
where our
values are
aligned with
our motives.
Many people
are stuck in
jobs they hate
and it’s
because of
values say
“well, you
should be
doing this”
and their
motives are
somewhere
else. Howard
Gardner, who
is at Harvard,
has done
research on
what he calls
"Good Work"
which is work
where people
are fortunate
enough to
align their
values, that
is their sense
of ethics,
with their
emotions, what
engages them,
and also what
they're good
at, their
excellence. So
when you align
excellence and
ethics and
engagement,
then you have
a calling that
you utterly
love. It may
or may not be
a paid job,
but it gives
your life the
most meaning
and is most
satisfying to
you.
Tricycle:
Is that like
self-actualization?
Daniel Goleman:
I would say
that’s an
ingredient in
self-actualization
and that
self-actualized
people find
their way to
that kind of
work or
calling.
Tricycle:
What in your
research is
exciting and
interesting
you at the
moment? What
are you hoping
people get
from your new
book? In
short, give me
a snapshot of
Daniel Goleman
right now.
Daniel Goleman:
Well, the
reason I did
this digital
book, The
Brain and
Emotional
Intelligence,
is that I
don’t stop
pursuing an
area once I
finished a
book about it.
I wrote
Emotional
Intelligence,
Social
Intelligence,
and
Working with
Emotional
Intelligence
but I've
continued to
be interested
in what
science can
reveal to us
about our
lives and
particularly
what the newly
emerging brain
science can
reveal to us.
My profession
is as a
science
journalist; I
was at The New
York Times for
a dozen years
before
Emotional
Intelligence
became a
career in
itself and I
continue to
try to harvest
scientific
findings that
are kind of
news we can
use that have
real
applications
to life. This
is extremely
satisfying to
me to continue
to share this
with others
who are
interested by
publishing a
shorter book
digitally and
to do it
quickly
instead of
setting aside
three years of
my life to do
a conventional
book. So, I'm
very happy
about this.
Back
to Genetics
Understanding
the
Amygdala in
Simple Language
by
the Website Author
Upon
many hours of
reading and
researching the
probable causes of
Borderline
Personality
Disorder….I saw that
there are two basic
reasons for
BPD: Genetics
and an
Invalidating
Environment in
a family of origin.
There are many
theories as to what
percentages are
attached to each of
the two
causes. This
brief discussion on
the Amygdala
concerns the Genetics
of what actually is
anatomically
resides inside
a BPD’s brain.
The Amygdala
(actually there are
2, so the Amygdalae)
are small
almond-shaped organs
in the brain—a left
amygdala and a right
amygdala. This
area of the brain
plays a major role
in memory recall,
responses to
stimuli, and
emotional regulation
with the outcome of
flight, fight, or
freeze responses.
It is agreed upon
that this organ is
part of our
instinctive and
reactive brains.
Stimulating the
amygdala
electrically (in
studies) creates
anxiety all the way
to panic and
fear. Much
information has
tried to convince us
that amygdala
reaction will cause
aggressive
behavior. This
is not necessarily
true. The
amygdala can produce
a hyper-sensitivity
to emotional
arousal.
The amygdala
will enable us to
vividly remember a
stressful event,
because of the
release of
adrenaline.
Adrenaline will aid
in highly accurate
recall of a
traumatic happening,
and actually put the
body into a similar
physical state
experienced as if
the event was
happening. The
feelings of
the memory are thus
stored along with
the facts of
the event.
Often times, panic
and anxiety will
cause the brain to
jump to inaccurate
conclusions of “what
is.” The brain
then focuses on the
possible threat or
dangers of harm or
death.
Men’s RIGHT amygdala
has a stronger
connection to the
brain, which keys
off their external
environment.
Women’s LEFT
amygdala has a
greater connection
with the rest of
their brain, and the
focus is normally
internal thought,
not external
environment.
It has often
been said that
Borderline
Personality Disorder
could be “a
perception
disorder.” And
who does the
internalizing of
perceived imminent
danger? Women
do. That is
why the largest
percentage of
Borderlines are
female. This
has been the belief
up to the most
recent decade, but
the numbers,
percentages and
identifiable
diagnoses have
changed. A lot
more men have been
diagnosed with the
disorder.
Also, the amygdala
has been found to be
smaller in
people diagnosed
with BPD. This
is a second
component to the
genetic cause of
BPD.
We have learned in
more recent years
through extensive
studies, that the
black and white
reasons and criteria
for BPD in either
gender has become
more grey in
color. The
genetic causes of
BPD in people, still
has an identifiable
physical component
(the amygdala’s size
and gender) along
with the environment
factor.
Women and men
perceive things
differently….even
their invalidating
childhood
environments.
The point here is,
this small pair of
organs has a very
prominent place in
the discussion of
the reason that BPD
manifests itself in
someone.
Back
to Genetics
Experience
Your Anger - Then Let it Go
Individuals working through a
borderline personality
disorder relationship should
be cautious not to spend
excessive time and energy in
the outer directed stage.
Everyone
passes through these stages in
their own way, and anger is
often a necessary release and
part of the natural grieving
process. But it is important
not to indulge one's self or
become consumed by anger to
the exclusion of moving
forward.
You
must move past the anger if
you desire to take control of
your life. ~
Facing The Facts
Back
to Relationship Recovery
Top
|
| Borderline
Personality
Disorder Label
Creates Stigma
|
by
Elizabeth
Bogod |
|
What's
in a name? In
the
disability
community this
question is a
hot topic. In
fact, the use
of negative
language has
proven time
after time to
be a major
influence on
individual and
public
attitudes
towards people
with
disabilities
and as Dahl
asserts often
constitutes "a
major barrier
for people
with
disabilities".
However,
despite
progress being
made to use
less
stigmatizing
disability
terms,
psychiatry
has not kept
up with these
changes.
Borderline
Personality
Disorder,
listed in the
Axis II
section of
Diagnostic and
Statistical
Manual (DSM
IV), is an
example of one
such term and
the focus of
this paper.
The DSM IV
defines BPD as
"a pervasive
pattern of
instability of
interpersonal
relationships,
self-image,
and effects,
and marked
impulsivity
beginning by
early
adulthood
...". The
mental
health
disability
causes extreme
emotional
vulnerability,
an unstable
sense of self,
impulsiveness
in potentially
self-damaging
behaviors
(e.g.,
spending, sex,
substance
abuse,
driving,
eating, etc.),
suicidal or
self-mutilating
behavior,
chronic
feelings of
emptiness,
intense anger
or difficulty
controlling
anger, and
periods of
feeling
removed from
reality
(dissociation).
This
paper will
discuss the
negative
connotations
of the term
"BPD", examine
the origin of
the term, the
effects it has
on treatment
and ways the
term shapes
both
individual and
public
perception of
people
diagnosed with
the disorder.
In addition,
the paper will
explore
whether or not
the term is an
acceptable use
of language
based on
current
terminology
standards
outlined in
the government
publication
"Worthless or
Wonderful".
Finally, it
will propose
recommendations
for changing
the name and
identify
recent
progress
towards this
goal.
Origin
The
origin of the
term "BPD"
dates back to
the early
1900's. At
this time
people with
mental health
disabilities
were either
categorized as
neurotic or
psychotic.
As it became
increasingly
clear to Dr.
Stern (an
early
psychiatrist)
that a growing
patient body
did not quite
fit into these
oversimplified
diagnostic
categories of
the day, the
term
"borderline"
was born.
According to
Dr. Stern's
theory, such
patient's
teetered on
the
"borderline"
between
neuroses and
psychoses.
Although this
theory went
out of favor
shortly after
it was
proposed, the
"borderline"
label stuck.
Inaccuracy
Dr.
Leland Heller
(M.D), an
expert in BPD
treatment,
believes the
BPD term is
inaccurate and
that the 'BPD'
label "in and
of itself is
as if the
whole person
(and the
personality)
is flawed
...". He
strongly
objects to
this
implication
because the
most recent
research on
BPD indicates
that the cause
of the
disorder is
not a "flawed
personality"
but rather a
biologically
based brain
disorder. He
believes there
is a
dysfunction of
the limbic
system of the
brain. Heller
backs up his
objection to
the term with
recent
research on
the biological
components of
BPD.
Another
study by Paul
Soloff, M.D.
and his
associates
found a
connection
between BPD
and low level
brain activity
in the
pre-frontal
cortex. Using
Positron
Emission
Tomography
(PET) scans,
researchers
can measure
glucose
levels
to detect
brain activity
Low glucose
levels have
been connected
to
deficiencies
in
serotonin,
a naturally
occurring
chemical in
the brain that
helps regulate
emotion. In
this study,
Soloff
established
two groups.
The first
group
comprised of
BPD patients,
while the
second group,
served as the
control group
made up of
participants
with no
history of
mental
illness.
Subjects from
both the BPD
group and the
control group
were either
given the
serotonin-enhancing
drug,
Fenfluramine
or a placebo.
Under both
conditions,
researchers
consistently
observed
higher
level
glucose
activity in
the frontal
lobes of
control
participants
than those in
the BPD group.
These
biological
explanations
for BPD
substantiate
Heller's
belief that
BPD is in fact
a biological
disorder, and
not just a
personality
flaw.
Dr.
Marsha
Linehan,
Ph.D., another
leader in the
field of
Borderline
Personality
Disorder,
proposes that
the condition
is a problem
with emotional
dysregulation.
Linehan
pioneered the
development of
Dialectical
Behavioral
Therapy (DBT),
a
well-recognized
method of
cognitive
therapy in the
treatment of
BPD. Core to
the success of
this therapy,
is the belief
that BPD is a
biological
disorder
characterized
by heightened
sensitivity to
emotion and
increased
emotional
intensity.
Heller
has suggested
that name
"Borderline
Personality
Disorder" be
changed to a
more accurate,
less
emotionally
laden term. He
has proposed
the term
"Dyslimbia" .
To explain the
term he breaks
it down into
two parts. The
first part,
"Dys" is the
Greek for
"disorder"
while the
second part,
"limbia"
refers to the
limbic system
of the brain.
Put together
the term
refers to a
biological
disorder of
the brain's
limbic system.
However, more
research may
be necessary
to bring this
term into
general use.
The advocacy
organization,
TARA -
Treatment and
Research
Advancement
Association,
would like to
see the name
changed as
well.
"The
name BPD is
confusing,
imparts no
relevant or
descriptive
information,
and reinforces
existing
stigma. We
believe that
BPD should be
refrained onto
a
spectrum
of its core
components-impulsivity
and emotional
dysregulation."
They
believe that
"Emotional
Regulation
Disorder" or
"Emotional
Dysregulation
Disorder" have
the most
likely chance
of being
adopted by the
American
Psychiatric
Association
(APA).
Dr.
Joel Dvoskin
(Ph.D.) seems
to agree that
something most
be done to
remove the
stigma of the
"BPD"
diagnosis.
He highlights
the reality of
what the "BPD"
label does
when applied
to an
individual. He
stresses that
"not all
mental health
diagnoses
foster
treatment" and
goes on to
identify BPD
as a diagnosis
that "hurts
people very
much". He
dislikes the
term because
it so often
results in
sub-standard
treatment of
people
diagnosed with
the disorder.
For example,
mental health
professionals
often label
undesired
behaviors of
BPD clients as
"manipulative"
and in need of
punishment
Yet, no matter
how many times
punishment is
administered
it has no
effect on the
so-called
"manipulative
behavior". So
why persist in
"treating" a
patient's
condition with
the
reward/punishment
model when it
clearly does
not work?
Dvoskin
believes when
such futile
attempts fail,
it is easier
for the
professional
to blame the
patient for
lack of
response to
treatment or
worse, fault
the patient
for a lack of
moral
fortitude than
admit the
professional's
own
shortcomings.
In fairness,
one should
mention these
patients are
often regarded
as
"notoriously
difficult to
treat".
However, Dr.
Dvoskin
believes that
one of the
main reasons
these clients
are considered
so difficult
to treat is
that mental
health
professionals
take out their
frustration on
the patient,
label their
patients as
purposely
causing their
own grief and
blame their
patients for
not responding
to treatment.
He asserts
"apparently
the greatest
sin a patient
can commit is
the sin of
poor response
to
treatment...".
The
last area
needing
exploration is
whether or not
the term
"Borderline
Personality
Disorder"
meets
currently held
standards for
proper
language use
in referring
to people with
mental
illness. The
report
"Worthless or
Wonderful"
recommends
that language
which
"suggests
negative or
judgmental
connotations"
be
changed to
more objective
terminology.
As mentioned
above, the
term
"Borderline
Personality
Disorder"
suggests the
judgmental
connotation
that the
personality of
the individual
is flawed.
Since
personality is
commonly
viewed as the
essence of who
we are, the
inference of a
flawed
personality is
very
insulting.
Therefore,
according to
the latest
recommendations
on proper
language use
in referring
to a persons
with
disabilities,
the term BPD
does not meet
current
standards.
In
light of the
out-dated, out
of favor
theory used to
develop the
"borderline"
label, the
negative
effect of this
label on
treatment and
patients
themselves,
and the
failing grade
given to the
BPD term based
on recognized
disability
terminology
standards,
surely it is
the duty of
every
professional
to explore the
inaccuracy of
the "BPD"
label and its
stigmatizing
effect on
those
diagnosed.
Needless to
say, the
people who are
most affected
by the stigma
of the "BPD"
label are
those
diagnosed with
the disorder.
Therefore,
those
diagnosed with
"BPD" can also
have a major
influence on
the use of the
term by
refusing to
accept it. As
"consumers" of
mental health
services, such
individuals
can empower
themselves by
speaking out
about how they
are affected
by the "BPD"
label and how
it affects the
mental health
services they
receive.
Acting as
their own
mental health
advocates,
people
diagnosed with
BPD can make a
difference to
change public
perception
about their
disorder and
make services
more adaptable
to their
needs.
Now
is the chance
for people
diagnosed with
BPD, concerned
community
members and
mental health
professionals
to speak out.
TARA is
encouraging
people to use
a copy of
their form
letter or
write their
own letter to
the APA to
express
support for
TARA's
advocacy
efforts (see
Appendix).
Through
expressing
these
concerns, the
APA will hear
the voice of
the people and
hopefully, in
the next
publication of
the DSM, do
away with the
stigmatizing
"BPD" label
altogether.
|
Back to Stigma
of Mental Illness & BPD
|
|
Despite Deeper
Understanding of Mental Illness,
Stigma Lingers
By Whitney
Blair Wyckoff
Even
though most people understand
that mental illness is caused by
brain biology, it still carries
a stigma. Knowledge is
power. And while some research
suggests that emphasizing the
science behind mental
illness—that it’s a brain
disorder and not a defect in
character—could be powerful
enough to help shake the stigma
around the condition, a recent
study in the American Journal of
Psychiatry found that tactic
isn’t paying off all that well.
Other researchers have found
that while more people
understand that mental illness
is caused by brain biology, it
hasn’t necessarily translated
into a decrease in
stigmatization. “We’re not
saying that the ‘disease like
any other’ line is going to
fail, but it’s taken us as far
as it's going to take us,” says
Bernice A. Pescosolido,
lead author of the study and
director of the Indiana
Consortium for Mental Health
Services Research.
Pescosolido and colleagues
analyzed how people responded to
questions about vignettes
describing people living with
schizophrenia, major depression
and alcohol dependence.
The data, from 1996 and 2006,
came from General Social
Survey. Researchers found
that 67 percent of the nearly
2,000 adults surveyed attributed
major depression to
neurobiological causes—up from
54 percent 10 years before.
Looking at schizophrenia, 86
percent of those surveyed
connected the disease with brain
biology, which is 10 points
higher than a decade earlier.
And the same figure for alcohol
dependence rose to 47 percent
from 38 percent. Also, there was
an across-the-board increase in
those who recommended medical
treatment for people living with
mental illness.
However, there was no
significant change in stigma
indicators. For example, 62%
indicated an unwillingness to
work closely with someone with
schizophrenia. And 74% said the
same for people with alcohol
dependence. How come? Many
people see mental illness as
something that never goes away.
“When you attach a feeling of
permanence to this, then it
justifies, in some ways, a
person’s sense of ‘otherness’ or
‘less-than-humanness,’”
Pescosolido says. She
adds, “There’s something about
the mind that people have a
different reaction to than body
affliction.”
Pescosolido is currently
researching how the stigma of
mental illness in the U.S.
compares to that in 17 other
countries. She says she hopes
the research will continue to
shed light on how to address
mental illness stigma.
Back to Stigma
of Mental Illness & BPD
|
Transference Focused
Psychotherapy Explained
in Human Terms
-With
Dr. Frank Yeomans; as
told by Tami
Green and adapted
from her article.
Dr.
Yeomans (Clinical
Associate Professor of
Psychiatry at the
Weill Medical College
of Cornell University)
developed
a special interest in
treating Borderline
patients during his
residency in the early
80's. Though the
(misguided) consensus at
the time was that BPD
patients were generally
difficult, he felt they
could be particularly
rewarding to work with.
Dr. Yeomans was asked
how TFP differs from
Dialectical Behavioral
Therapy (DBT), the most
well-known treatment
option for BPD here in
America, and he offered
this example:
"When a
patient has a hard time
getting a job, and tends
to get anxious and angry,
tends to feel she is being
challenged, she responds
in a hostile way. DBT will
teach her to master the
reactions, while TFP
questions her perceptions
and helps her distinguish
between the internal and
external reality.
TFP helps
sort out the internal
perceptions that stem from
childhood that may not
match the external reality
of today. It helps the
patient question the way
they think. In order to
accomplish this, these
therapists don't soothe
their patients, so that a
natural relationship is
developed."
In this way,
feelings that would
normally arise in the
course of a relationship
are felt during therapy so
they can be thought about
and discussed.
Dr. Yeomans
was asked "it is possible
to assist someone in
changing their internal
view?" He
said, "by validating and
then challenging. Get them
to think. It may take
months and years of going
back and forth. As a
therapist, you can
introduce data into
someone's mind so they can
begin to entertain it, but
it only lasts a while
because it usually feels
safer to return to the
previously held position."
When asked
about actually changing
the brain neurobiology, he
offered some very exciting
news: "There is more
plasticity in the brain
than once believed. The
change happens through
repetition, exposure and
reflection." It would only
make sense that to change
our brain permanently
would take a lot of time,
then. However, life is not
put on hold during
therapy.
As a matter
of fact, engaging in the
world is a very important
requirement of the
therapy. Repetitive bad
outcomes of the past--such
as failed relationships or
jobs--can be turned around
successfully by bringing
the real-time challenges
to the therapy where they
can be discussed and
worked through. And though
two therapy sessions are
held each week, more than
that is discouraged, as it
fosters a dependence upon
the therapist that is
unnecessary.
He also
discussed how TFP is a
little controversial
because of its' emphasis
on the basic nature of the
two sides of the human
mind: the loving side
(affinity and affection)
as well as the competitive
aggressive side.
Dr. Yeomans
continued by saying:
"Our
Mentalization (MBT) and
DBT colleagues don't talk
about innate aggressive
drives, but even though
these drives have been
tamed in civilization,
what do we do with them
now? Part of TFP is
integrating the aggression
and mastering it."
Speaking of
this aggressive side and
the need to integrate it,
he added, "it was once
thought that more women
than men had BPD, but we
now know that it is an
equal percentage of each.
It's just that more men
with BPD show up in jail,
not in the clinical
community."
He said that
everyone has this
aggressive side, not just
those with BPD. TFP helps
the patient to learn to
stop and analyze
reactions. There is, for
example, nothing wrong
with yelling and screaming
if you chose to do it and
control it and use the
behavior effectively.
Back to TFP
Top
|
Do
Deficits in
Mindfulness
Underlie
Borderline
Personality
Features and Core
Difficulties?
by
Michaelsweiss
From
Biology Magazine
Forums
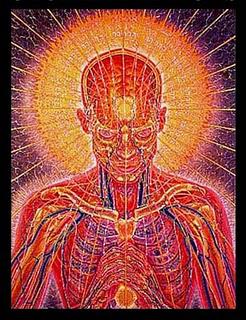
Review of
Study
Published in
the
Journal of
Personality
Disorders
Previous
research
includes several
different models
to identify the
core mechanisms
responsible for
the diverse
features
associated with
Borderline
Personality
Disorder.
This disorder
presents with a
variety of
features that
include
ineffective
interpersonal
skills and
emotion-regulation
dysfunction.
Individuals
diagnosed with
Borderline
Personality
Disorder
typically have
issues related
to awareness,
attention, and
self-acceptance. Most
previous
research
regularly
associates
mindfulness with
the presentation
of many of these
issues; but
there is limited
research
exploring the
correlation
between
mindfulness and
Borderline
Personality
Disorder
symptoms.
The purpose of
this study was
to observe
whether, in
fact,
mindfulness
deficits
underlie the
broad areas of
dysfunction
commonly
associated with
the clinical
features of this
disorder.
To do this, the
authors examined
the relationship
between
mindfulness
deficits and a
diverse
non-clinical
sample that was
representative
of a wide range
of Borderline
Personality
features.
The authors tested
three main
hypothesis based
on the empirical
evidence of
previous
research.
The first
hypothesis was
that there would
be a negative
association
between
mindfulness, and
the core areas of
dysfunction of
Borderline
Personality
Disorder.
The second
hypothesis
predicted that the
association
between
mindfulness and
these clinical
features would be
statistically
significant when
controlling for
neuroticism.
The final
hypothesis was
that mindfulness
would be able to
predict Borderline
Personality
Disorder features
beyond its
associations with
the regular
functioning of the
features
associated with
this
disorder.
The sample used
for this study
consisted of 342
undergraduate
students who
were currently
enrolled in an
introductory
psychology
course at the
University of
North Texas.
Mindfulness
was measured
using a fifteen
item,
Likert-type
scale known as
the Mindfulness
Attention
Awareness
Scale.
This scale
assesses several
different traits
that are
characteristic
of mindfulness
including
aspects of both
attention and
awareness.
Borderline
Personality
Disorder
features were
assessed using
both self-report
scales and
written response
items. Neuroticism
was also
assessed due to
its high
correlation with
Borderline
Personality
Disorder.
This was
accomplished
using a six
item,
likert-type
scale that
assessed the
tendency towards
negative
emotions.
The results of
this study
indicate that
mindfulness is
positively
correlated with
interpersonal and
emotional
functioning, and
negatively related
to the
dysfunctional
emotional and
interpersonal
features
associated with
Borderline
Personality
Disorder.
Although weaker;
the negative
correlation with
Borderline
Personality
Disorder remained
statistically
significant when
controlling for
neuroticism.
Analysis of data
suggests that
mindfulness
significantly
predicts
Borderline
Personality
Disorder beyond
the effects of
features common to
the disorder. This
research suggests
that the
dysfunctional
features of
Borderline
Personality
Disorder may be
explained by
problems related
to mindfulness
combined with
features of
neuroticism.
Mindfulness was
indicated as a
main construct for
explaining the
primary areas of
dysfunction common
to Borderline
Personality
Disorder.
One
limitation of
this study was
the use of
undergraduate
psychology
students to
comprise the
sample.
This may
indicate a
limited ability
to generalize
results to
clinical
populations.
Another
limitation is
the inability to
draw causal
conclusions due
to the
co-relational
design of the
study. The
relationship
between
mindfulness and
neuroticism must
be studied
further in order
to understand
the direct
effects of each
variable on
Borderline
Personality
Disorder
features.
This study was
meticulously
designed and
analyzed using
strict data
analysis
procedures. The major
problem with
this study is
the inability to
isolate all
independent
variables.
This is not a
reflection of
faulty
methodology, but
an indication of
the complex
clinical
presentation of
features related
to this
disorder.
This problem is
most likely
characteristic
of all clinical
studies that
attempt to
broadly examine
Borderline
Personality
Disorder.
This study has
broad implications
for future
research and
clinical
work. I am
interested in
understanding how
mindfulness
meditation can be
positively
utilized in
clinical
application.
The relationship
between
mindfulness and
Borderline
Personality
Disorder suggests
that future
research involving
mindfulness
meditation may be
warranted.
It would be
interesting to see
if the
introduction of
mindfulness
meditation would
increase the
efficacy of
current
therapeutic
models.
Top
|
|
The
STEPPS Group Treatment Program
for Borderline Personality
Disorder directly from the
steppsforbpd website;
STEPPS
is the Trademark of: N.S.
Blum, N.E. Bartels, D. St.
John, B. Pfohl, 2002. All
rights reserved.
Introduction to Training
The
Iowa program began in 1995, and is
based on a systems approach to
treatment of individuals with
Borderline Personality Disordered
(BPD) originally developed by
Bartels and Crotty (1992). That
program has subsequently been
adapted and revised by Blum, St.
John, and Pfohl (2002). The
current program includes two
phases--a 20-week Basic Skills
group, and a one-year,
twice-monthly advanced group
program called STAIRWAYS. The
combined program is identified by
the acronym STEPPS, which stands
for Systems Training for Emotional
Predictability and Problem
Solving.
In
this cognitive-behavioral, skills
training approach, Borderline
Personality Disorder (BPD) is
characterized as a disorder of
emotion and behavior regulation.
The goal is to provide the person
with BPD, other professionals
treating them, and closely allied
friends and family members with a
common language to communicate
clearly about the disorder and the
skills used to manage it. Clients
learn specific emotion and
behavior management skills. Key
professionals, friends, and family
members whom clients identify as
part of their “reinforcement
team,” learn to reinforce and
support the newly learned skills.
This helps avoid the phenomenon of
“splitting,” a process in which
the person with BPD may
externalize their internal
conflict by appearing to draw
others around them into taking
sides against each other and
arguing out the merits of
differing perspectives and
behaviors. Splitting, like other
behaviors common in BPD, is viewed
not as an intentional act of
aggression, but as an automatic
response to the emotional
intensity and dysregulation which
the client can learn to anticipate
and replace with more effective
behavior.
Underlying
this training approach is the
assumption that at the core of BPD
is an actual clinical entity, a
disorder that might be
characterized as a defect in the
individual’s internal ability to
regulate emotional intensity. As a
result, the person with BPD is
periodically overwhelmed by
abnormally intense emotional
upheavals that drive him or her to
seek relief. Family studies
suggest an underlying biologic
vulnerability. The childhood
history of the person with BPD
often includes inconsistent
emotional support or even abuse by
important caregivers. In most
cases there is a complex interplay
between underlying vulnerability
and the social environment.
Identifying someone to “blame” for
the disorder is usually
counterproductive. We believe that
individuals with BPD do not
consciously choose to have this
disorder and, with rare
exceptions, parents and other
important caregivers do not
consciously choose to create an
inconsistent and unsupportive
childhood environment.
Early
in treatment, many of our clients
view the term personality disorder
as a code for, “it’s all your own
fault.” The term borderline seems
to imply that it is only a matter
of time before they fall
completely “over the edge.” For
these reasons, clients often
resist the label of BPD, even
though they may readily
acknowledge the behaviors. Bartels
and Crotty have suggested the name
Emotional Intensity Disorder as a
more accurate description that
clients find easier to understand
and accept. We use both terms
interchangeably. Regardless of the
terminology, there are significant
advantages to reframing one’s
understanding of BPD as a
disorder. Rather than viewing
themselves as someone who is
attempting to manipulate, is
attention-seeking, or is
sabotaging treatment, the trainees
learn to view themselves as driven
by the disorder to seek relief
from a painful illness through
desperate behaviors which are
reinforced by negative and
distorted thinking.
The
training is composed of three
steps:
Step
1 - Awareness Of Illness
The
first step for the client is to
replace misconceptions about the
BPD label with an awareness of the
behaviors and feelings which
define the disorder. Behaviors can
be changed and feelings can be
managed. Clients often begin with
the belief that they are fatally
flawed (for which they may
alternately blame themselves or
others) and that they deserve to
suffer. The ability to entertain
the notion that this is a
legitimate illness and that the
individual can learn specific
skills to manage it is an
important precursor to developing
the capacity for change.
Clients
are provided with a printed
handout listing the DSM-IV
criteria for BPD and time is
provided for trainees to
acknowledge examples of the
criteria in their own behavior
(“owning” the illness). A second
component is the concept of
cognitive filters. Therapists may
recognize the similarity to the
concept of schemas described by
Jeffrey Young (1999) in Cognitive
Therapy for Personality Disorders
– A Schema-Focused Approach. A
questionnaire has been developed
to allow trainees to identify
their early maladaptive filters
and to see the relationship
between these filters, the DSM-IV
criteria, and their subsequent
patterns of feelings, thoughts,
and behaviors.
Step
2 - Emotion Management Skills
Training
We
describe the five basic skills
that aid the person with BPD in
managing the cognitive and
emotional effects of the illness.
Combined with an understanding of
how the illness works and
recognizing the filters that have
been triggered in a given
situation, the skills assist the
person with BPD in predicting the
course of an episode, anticipating
stressful situations in which the
illness is aggravated, and
building confidence in their
ability to manage the illness.
Step
3 - Behavior Management Skills
Training
There
are eight behavior skills areas
the person with BPD must work at
mastering. As the BPD syndrome
progresses through the disruptive
interplay between the emotionally
intense episodes and a social
environment that becomes
increasingly unempathic and
unresponsive, many functional
areas may begin to break down.
Learning or relearning patterns of
managing these functional areas
helps the person with BPD to keep
these areas under control during
episodes.
STEPPS
Basic Skills Group Program
The
Basic Skills Program consists of
20 weekly meetings of two hours
each. This includes a short break
between the first and second hour.
Each week is organized around a
skill which is the focus of the
session. Some skills require more
than one weekly session to teach.
The skills include:
•
Distancing • Communicating •
Challenging • Distracting •
Managing Problems • Setting Goal •
Eating • Sleeping • Exercise •
Leisure • Physical Health • Abuse
Avoidance • Relationship
Management
For
those groups whose meetings occur
during the Holiday Season, we have
included an optional unit (See
Appendix) on managing emotional
intensity during this time of the
year.
Outpatient
Treatment - Classroom “Seminar”
Format
The
training format is a weekly
two-hour classroom experience with
two trainers and 6-10 trainees.
Trainees are supplied with a red
notebook in which to keep their
training materials. They are
instructed to bring in the
notebook to each session. They are
strongly urged to share their
notebook and the lesson materials
with others in their system. By
the end of the training, most
clients view the red notebook as a
resource they can turn to during
difficult times.
Rather
than following a traditional group
therapy model, sessions have the
look and feel of a seminar.
Clients sit at a conference table
facing a board. Besides the use of
the board and the printed
materials, the training is
facilitated by poetry, audio
recordings of songs, art
activities, and relaxation
exercises. It is not unusual for
clients to bring in materials,
poems, and even art work they have
created that reinforce the skills
and themes of the meetings.
A
typical class session begins with
trainees completing the Borderline
Evaluation of Severity over Time
(BEST) form, which allows them to
rate the intensity of their
thoughts, feelings, and behaviors
over the past week. They keep
track of their weekly score on a
graph. This allows them to see the
variability that is typical of
BPD, and to note over time the
decrease in the intensity of their
emotional episodes and the
increased use of the positive
behaviors and skills being taught.
The BEST can be used for data
collection to evaluate the
effectiveness of training. The
data will allow monitoring of
increases and decreases in
self-abuse urges and behaviors, as
well as emotional intensity,
negative behaviors (e.g.,,
substance abuse, eating-disordered
behavior), and positive behaviors
(e.g., choosing a positive
activity, keeping appointments,
etc.). This is followed by a brief
relaxation/observation exercise.
Scripts for some of the activities
are written out and available in
the handouts. Participants are
encouraged to record the scripts
(e.g., for progressive muscle
relaxation and visualizations) to
use outside of the sessions.
The
first half of each session is
spent reviewing the Emotional
Intensity Continuum, which
operationalizes the concept of
varying degrees of emotional
intensity on a 1-5 scale. A 1 is
feeling calm and relaxed, and 5 is
feeling out of control, engaging
in self-destructive impulses,
angry outbursts, etc. Clients are
expected to fill this out on a
daily basis and to summarize the
per cent of time spent at each
level during the previous week.
Clients often achieve a more
balanced view of themselves
through this self-rating. In
addition, clients are often
surprised to find that they do
have significant periods of time
when they are not at the highest
level of emotional intensity.
The
authors gratefully acknowledge the
contribution and creativity of
Cynthia Claude-Rawson for her
artistic conceptualization of the
Emotional Intensity Continuum
(please refer to week 1), and her
illustrations and poems in the
lesson on Eating Behaviors (week
15).
A
Skills Monitoring Card lists the
skills being taught and allows
trainees to indicate which skills
they used in the previous week. As
part of the family/caregiver
education component, clients are
encouraged to give an abbreviated
version of this card to members of
their reinforcement team. The
previous week’s homework
assignment(s) are reviewed and the
remainder of the session is
devoted to introducing the
material for the current lesson.
Participants are encouraged to
read aloud the material being
introduced
With
occasional exceptions, our clients
take to this structured approach
to emotional problem solving very
well. On one occasion when a group
leader was unexpectedly delayed
about 20 minutes, she arrived to
discover that the group had
appointed one of the members to be
the leader and the group was well
into reviewing the Emotional
Intensity Continuum for the group.
In the advanced (STAIRWAYS) group,
clients regularly request
permission to conduct that portion
of the session.
While
in a training session, a person
with BPD may try to reframe their
emotional experience in the
context of or as a result of some
personal or interpersonal problem.
While there is an opportunity for
clients to respond and share
experiences relevant to the skills
being taught, the structure does
not allow the group to spend long
periods of time focusing on a
given group member who may be in
crisis. One effect of the
structured format is to model how
to acknowledge problems and offer
support while still imposing
reasonable limits and boundaries
on the scope of interaction so the
main goal of the meeting is not
lost. The group leaders must be
prepared to re-reframe problems in
the context of the disorder and
filters. The rule to use is: focus
on the disorder, not the content.
The
Systems Component of STEPPS
Whether
it is cause or effect, the
individual coming to therapy is
usually enmeshed in a system of
relationships in which even
concerned and well-intentioned
friends and significant others
respond to the individual with BPD
in a manner that reinforces
pathologic behavior. For example,
the individual experiencing a
perceptual distortion that others
dislike him or her may become
irritated and behave in ways that
turns the distortion into a
reality. This new reality then
serves to reinforce the cognitive
distortions and maladaptive
behavior.
For
20 weeks, the STEPPS group becomes
a mini-system in which the trainee
receives instruction on new ways
of thinking and new behaviors.
Trainees receive positive
reinforcement in the form of
support from group trainers and
other group members. The new
behaviors are designed to
influence the individual’s larger
support system so it too begins to
reinforce healthy behavior.
It
helps if everyone uses a
consistent approach and language.
The group has also proved to be a
very successful training vehicle
for other professionals who have
then gone on to start their own
STEPPS groups in other locations.
STEPPS emphasizes that the
trainees can and should take
responsibility for taking steps to
help key players in their system
respond more effectively.
Specifically, STEPPS incorporates
the following 4 components to
address the trainees support
system:
1.
Teaching the trainee to challenge
cognitive distortions and to
develop more realistic
expectations about what types of
support are appropriate from key
players in their support team.
2.
Teaching the trainee a series of
strategies for dealing with
anxiety, anger, depression, and
self-destructive thoughts which
can be accomplished either
independently or with a level of
input from others that the support
system can comfortably provide.
3.
Encouraging the trainee to share
appropriate sections from their
red manual with close friends and
significant others (as well as
her/his other mental health
providers) so that these
individuals can better understand
the illness, the terminology, and
ways of responding to the trainee
that reinforce the strategies
taught in the STEPPS program.
4.
Offering two special evening
sessions in which key members of
the support team are invited to
come and learn about BPD, how
STEPPS works, and what they can do
to help. We provide written
guidelines that summarize how to
respond to the trainee on
occasions when the trainee is
feeling desperate and out of
control.
Integrating
STEPPS With Other Treatments
Clearly,
STEPPS is not a comprehensive
treatment program for managing
individuals with borderline
personality disorder. From it’s
inception, STEPPS was designed to
be a “value added” treatment
intervention which augments rather
that replaces the existing network
of mental health providers. This
approach helps reduce the time and
expense needed to set new STEPPS
treatment groups. STEPPS has been
implemented in a wide variety of
settings and is usually well
received by other providers who
continue to provide mental health
services to individuals enrolled
in STEPPS
Clients
in the STEPPS program are
frequently being treated with one
or more psychopharmacologic
agents, most often antidepressants
and mood stabilizers. The program
addresses compliance with
medications as prescribed by the
client’s physician as an important
enabling factor for the group
therapy program. Substance abuse
is viewed as treatment disabling
and clients are required to seek
appropriate substance abuse
treatment and maintain abstinence
either before or concurrently with
the STEPPS program. Clients with a
severe eating disorder are
similarly required to be in an
appropriate treatment program.
Trainers
should note that in the
development of this treatment
approach, the need for traditional
individual therapy may be reduced.
In fact, a team approach to
working with a person with BPD who
is familiar with the skills and
behavior patterns has been found
by Bartels and Crotty to be
preferable to an individual
approach. The optimal treatment
system is one in which, in
addition to the weekly skills
training, the person with BPD
receives skill and behavior
pattern reinforcement from all
treatment system personnel,
family, and friends. This approach
encourages the person with BPD to
rely on peers, family, and others
for reinforcement and reduces the
possibility that the person with
BPD will focus exclusively on a
single therapist who then runs the
risk of being alternately
over-idealized and devalued by the
person with BPD. Those individuals
receiving individual therapy are
eligible for the STEPPS program
provided the therapist agrees to
support the program by reviewing
the STEPPS materials with the
client as they add the lessons to
the red notebook each week. We
provide several opportunities for
professionals, relatives, and
significant others to participate
in the program. During the 20
weeks, a special evening session
is held that also includes
professionals, relatives, and
significant others. In addition,
we have found that the clients are
quite willing to have significant
others and even their individual
therapist attend a regular group
meeting, and group members are
given permission to bring them to
any two sessions following the
evening session.
Top
|
|
What
Borderline in a Parent Can
Do to the Family Members,
Especially the
Complications
in Children
from
http://mrstreasures.wordpress.com

St. Dymphna is the patron
saint for emotional
disturbance
Veronica,
a reader of my article
“Mother’s Day and
Borderline Personality
Disorder: When your Mom is
an Emotional Terrorist”
articulated in her own words
the pain
“Thank-you
for telling the real truth
about how difficult it is
and how utterly
emotionally draining it is
to have a mother with
borderline personality
disorder. There are so
many articles that tiptoe
around the truth and never
tell how adult children of
BPD’s are in constant
terror from their mothers.
This article was spot-on
and I thank-you for giving
a voice to all the adult
children who are utterly
confused and victims of
this terrible illness that
rips families and souls
apart. I am an adult child
victim as well and I could
relate to EVERY sentence
in this article.
Veronica (2008, May 05)
“When
your Mom is an Emotional
Terrorist” is
about the plight of
children and their
relationship with their
Borderline mother.
They love her so much
but being children, it is
very hard for them to
understand the difference
between the illness and
their mother’s behavior.
There seems to be no
demarcation line that their
mother is now being
BORDERLINE. The
emotional outbursts are very
unpredictable and scary for
them. Their world used
to be very chaotic, their
inner disturbances are acted
out in other behaviors.
It leads me to the
question if we should protect
the children of BPD mothers?
How will we do it?
Do we let them suffer
their fate?
The
spouses of Borderlines are
so engrossed with the
partner’s never-ending
problems that many children
needs are emotionally
neglected. The spouses
are suffering from Post
Traumatic Stress Syndrome
(PSTD) themselves and trying
to make sense of their
miseries. The children are
suffering from Development
Trauma Disorder (DTD) and
possibly Reactive Attachment
Disorder.
A facade of
normalcy is displayed to the
outside world. But in reality,
these children live in
self-contained prison camps.
Some through genetic
disposition end up being
Borderline. Some are
able to make a drastic effort
not to be Borderline.
But everyone in the
process is traumatized.
BPD is a disorder that
should not be taken lightly.
If you are in a BPD
relationship and your partner
is in denial, please protect
your innocent children.
Each day in a BPD
relationship is deadly for a
child. Think of your
children.
(More)
Complications
of BPD
from MedicineNet.com
website
What
are borderline personality
disorder complications?
The presence of
BPD can often worsen the
course of another mental
condition with which it
occurs. For example, it tends
to change the symptoms of
posttraumatic stress disorder
and to worsen depression.
Individuals with
BPD are at risk for
self-mutilation, as well as
for attempting or completing
suicide. While both
self-mutilating and suicidal
behaviors seem to be
associated with alleviating
negative feelings, it is
thought that self-mutilating
behaviors are more an
expression of anger, punishing
oneself, distracting oneself,
and eliciting more normal
feelings. In contrast, suicide
attempts are thought to be
more often associated with
feeling survivors will be
better off for their death.
People who engage in
self-mutilation are more
likely to commit suicide
compared to those who do not
self-mutilate.
Although most
individuals with a mental
disorder do not engage in
violent behavior, those who
suffer from BPD have a
somewhat increased risk for
such behaviors. That risk is
also increased for individuals
who suffer from antisocial
personality disorder, have
previous history of violent
behavior, frequent use of
sedative medications, or
experience several changes in
their psychiatric medications
in general.
Complications
of BPD also often involve
families of the person with
the disorder. For example, a
parent with BPD is
vulnerable to having
depressive symptoms in their
children.
Top
Personality disorders: One
of the most controversial
& misunderstood areas
of mental health
By Anthony Bateman
Notebook September, 14
September 2011
Ask the average person what
they associate with
personality disorders and you
get a blank stare or
description of a human
chameleon capable of changing
from normality to social
menace in the blink of an
eye.
In reality, the majority of
people with a personality
disorder are a greater danger
to themselves than others,
with high rates of self-harm
and attempted suicide as a way
of managing often turbulent
emotions.
Most of us recognize our moods
and feelings and manage them
until they pass, while many
people with personality
disorders have a tendency to
get stuck in these emotional
states which increase in
intensity, resulting in
behavior that many of us find
unusual.
These limiting patterns of
behavior and response become
engrained like a scratched
record, producing great
feelings of anxiety and
frustration.
Sadly, public perception of
the condition is largely media
driven with a succession of
sensationalist headlines,
films and books. These
inevitably focus on people
with antisocial personality or
psychopathic conditions which
are among eleven recognized
disorders.
There is no doubt that those
with severe psychopathic
traits are dangerous and prone
to criminal activity. This
is through
characteristics that include
impulsive self centered
behavior that puts their own
needs above others. However,
they are in a minority and
their impact on society is
greatly exaggerated and
dramatized in all but the most
extreme cases.
It
is somewhat ironic that that
the media’s highly
manipulative and attention
grabbing behavior itself
shows the collective
symptoms of a personality
disorder. They involve
showing signs of extreme
behaviors that we all
share, which is why we can
recognize and identify many
of the traits in ourselves –
albeit at a less amplified
level.
An interesting illustration of
this was a study by
psychotherapists in 2005 that
matched the personalities of
top British executives with
psychiatric patients at
Broadmoor Hospital. The
results found the two groups
had more in common than first
expected. This included
Histrionic Personality
Disorder, whose
characteristics include
superficial charm and
ego-centricity, Narcissistic
Personality Disorder, which
includes grandiosity and self
focused lack of empathy, and
Obsessive Compulsive Disorder,
reflecting excessive devotion
to work, dictatorial
tendencies and
perfectionism.
Of course, this should be
taken with a pinch of salt.
There are people who can
function with personality
disorders but they are rare,
and the severity of their
condition questionable.
In reality, diagnosed disorder
types have difficulty forming
or maintaining relationships,
meaning many are isolated by
unemployment and have
associated conditions such as
depression and anxiety.
So how common are personality
disorders? A sensible bench
mark is around 1% of the
population, with some of these
conditions being more common
than others, such as Obsessive
Compulsive Personality
disorder. These individuals
become fixated on orderliness,
cleanliness and being in
control, while those with
borderline personality
disorder have a poor self
image and often experience
feelings of emptiness,
depression and paranoia.
Although I’d be the first to
admit that diagnosis isn’t
straightforward as the
disorders often share
overlapping symptoms.
There has been much debate
about the stigmatization of
labeling people with
conditions, but I have found
patients and families often
find relief in finding
something tangible to get to
grips with.
Seeing more than 30 patients a
week in one-to-one and group
sessions, I primarily use one
of several ‘talking therapies’
I co-developed called
Mentalization. This teaches
patients to become more aware
of their own thinking and
learn to rationalize, manage
and understand their mental
states and emotions, as well
as those of others. Therapy
can take up to two years and
the good news is that the
majority of patients make a
significant or full recovery
through a combination of
talking therapy treatments
like ‘Mentalization’ and
‘Improvement with Age’.
Two of the biggest
challenges our profession
currently face are:
Firstly, discovering an
effective way of measuring the
severity of personality
disorders so we can plan the
duration and intensity of
treatment and its likely
long-term impact on mental
health services.
Secondly, we have to treat
people with these disorders as
a matter of course and that
calls for greater education
and awareness both in and
outside the health
service.
There are still incidences
where an as yet undiagnosed
patient may turn up at a GP
surgery or reception areas of
some NHS facility and be told
to leave the premises because
they are being difficult or
aggressive. Staff probably
don’t recognize the
possibility of an underlying
problem and that is something
that needs to be more widely
addressed so patients can be
quickly and effectively
signposted to the right
service.
Greater public awareness and
compassion are powerful tools
that can be used to give both
ourselves and those being
treated a greater insight into
personality disorders.
Top
|
|
|
Site-MapTop |
Site-Topics |
| General Information |
Brain chemistry, Legal system,
Characteristics Nat'l Alliance on Mental Illness,
Definition of BPD, Resource Center, Stories,
Pictorial diagram, Abandonment, Dual
diagnoses, Problems,
Solutions. |
| Blogs |
Body of site. |
| Books |
Body of site. |
| Causes |
Body of site. |
| Characteristics of BPD |
characteristicsofBPD.htm (link), sib.htm
(link); Self-injury, Suicidality,
Etc. |
| Comments from BPD's |
patientsspeakout.htm
(link),
BPD's tell it like it is. |
| Compulsion |
impulsive.htm
(link) |
| Contact Us |
Ask questions, address comments to me.
|
| Crisis
(handling a crisis) |
crisis.htm
(link)
Suggestions on what
to do when you may be in crisis-mode, or just
distresses |
| Discussion of BPD's and
Non's |
bpd&nondiscuss.htm
(link).
|
| DBT |
Body of site. dbtskills.htm (link) |
| DBT-certified Therapists |
Body of site.dbtskills.htm
(link) |
| DBT Resources &
Facilities |
dbtskills.htm
(link). |
| Dual Diagnoses |
Body of site; Borderline
with another mental illness or addiction. |
| EMDR |
Body of site; Eye
Movement Desensitization Reprocessing. |
| Function of Anger |
Body of site;
Function of anger is to stop stress. |
Help for Non-BPD's
|
tools4nonbpd.htm
(link), melodybeattiebooks.htm
(link), runonbpd.htm
(link), Books, Legal help, Support groups,
Techniques, Resources, Healthy Relationships; What
you can do for your BPD. Importance of the
hormone Oxytocin |
| How BPD Impacts Employment |
employment.htm
(link) |
| Impulsivity |
impulsive.htm
(link). |
| Interactive Forums |
BPD Tumblr, Yahoo Angry Heart Grp,
Self-help for SIB, BPD Central, BPD Haven, BPD
Resource Ctr |
| Living in Recovery |
Living your life after at least 2 years
of treatment: calming.htm |
| Marsha Linehan |
DBT, DBT Therapists, DBT & SIB,
P.L.E.A.S.E. linehan.htm |
| Medical Journal of CA |
33 doctors in this field, 84-page journal. |
| Media & BPD |
Hi-lited public figures with
BPD |
| Medications |
Anti-anxiety, Mood
stabilizers, Anti-psychotics, Anti-depressants;
medication.htm
(link). |
| Mentalization |
Body of site.
also, mentalization.htm
(link) |
| Mindfulness |
Body of site. |
| Movies |
Body of site. |
| Personal Blog of a
Borderline |
http://bpddailyjourney.blogspot.com .
(link) |
| Professionals |
Body of site; many, many links. |
| Proven Fact |
Comic relief; youneedthissite.htm
(link). |
| Recklessness |
characteristicsBPD.htm
(link); Characteristics listed, Videos, a Story. |
| Recovery from ADDICTIONS |
additionrecovery.htm
(link); Borderline often accompanied by
addiction. |
| Relationships with BPD's |
Recovery, Tami Green's story and site,
Relationship Stages, Discovery Stages for Family
Members |
| Reducing Severity of BPD |
Body of site. |
|
SCHEMA |
Body of site. See
also schema.htm (link) |
| Self-Injurious Behavior
(SIB) |
sib.htm
(link) Cutting, burning. |
| Special Thanks |
specialthanks.htm
(link); People who contributed directly or
indirectly to my recovery and this site. |
| Statistics |
Body of site; Statistics for BPD,
Alcoholics, Eating Disorders. |
| Stigma of Mental Illness |
By Others; By Professionals. |
| Suicide |
See Recklessness. |
|
Support Groups for
BPD's |
See Interactive Forums. |
| Treatments |
Medication, DBT, MBCT, TFP, MBT, Schema,
STEPPS, BASE, EMDR,
therapywhatworks.htm (link). |
| Treatment Centers |
Where they are; What they do. |
| Videos |
BPD Overview, Being Borderline,
Self-Harm (SIB), etc. |
| Writing |
Poems by Borderlines. writing.htm
(link) |
| Zen |
mindfulness.htm
(link). |
| Calming Mindfulness |
Miscellaneous readings to calm
yourself. calming.htm
(link) |
| Living with BPD |
livingwithbpd.htm (link). |
| Living
in Recovery and beyond |
Going beyond the skills/treatment of
BPD calming.htm
(link) (See "Readings & Positive
Person")
Also includes the page
positiveperson.htm. (link) |
| Conclusion |
conclusion.htm
(link) Summing it up. |
|
Lay-Persons |
laypeople.htm (link);
Pass this site on. |
|
Professionals |
professionals.htm
(link); Treat, don't avoid, BPD's within
your caseloads. |
| Top
Line 339 of source code to change the year |
|
|
|
| |
|
|

 Daniel
Goleman:
I think it's
an enormous
experiment
with our sense
of community
and our
children.
Evolution
designed the
human brain
for
face-to-face
human contact,
particularly
our capacity
for empathy,
which, of
course, is
very strongly
related to our
sense of
ethics.
Empathy is the
essential
factor for
compassion but
online we may
be disabling
this. The
social centers
of the brain
seem to act
like an
interpersonal
radar attuning
to the person
we're with,
and activating
in our own
brain what's
going on with
that
person—their
feelings,
their
intentions,
their
movements.
Because we
have this
inner sense of
what they're
doing we don’t
have to think
about it; this
is another
automatic
function.
Daniel
Goleman:
I think it's
an enormous
experiment
with our sense
of community
and our
children.
Evolution
designed the
human brain
for
face-to-face
human contact,
particularly
our capacity
for empathy,
which, of
course, is
very strongly
related to our
sense of
ethics.
Empathy is the
essential
factor for
compassion but
online we may
be disabling
this. The
social centers
of the brain
seem to act
like an
interpersonal
radar attuning
to the person
we're with,
and activating
in our own
brain what's
going on with
that
person—their
feelings,
their
intentions,
their
movements.
Because we
have this
inner sense of
what they're
doing we don’t
have to think
about it; this
is another
automatic
function.